Abstract
Abstract 1920
Understanding of leukemia biology and advances in the transplant field have improved the safety as well as access of allogeneic hematopoietic cell transplantation (HCT) for a larger number of patients (pts) affected by acute myeloid leukemia (AML). The trend of growth of HCTs in adult pts with AML can be expected to continue based on acceptance and availability of alternative donor. Few data are available for: i) the reliable estimates of the number of HCT for AML and the total number of AML pts for whom HCT is appropriate, ii) the choice of the different donor sources.
A risk-adapted treatment strategy is crucial to improve the outcome of pts with AML. Our policy is to offer a haploidentical HCT to adult pts lacking a matched donor in the appropriate time according to clinical indications (www.leukemianet.org, www.ebmt.org). This policy is integrated in ongoing protocols for primary disease (www.nilg.it).
Here we are reporting the intention-to-treat (ITT) analysis of HCT in all consecutive AML pts referred to our Institution between January 2004 and April 2012. Classification, prognostic evaluation, response criteria and survival outcomes for AML were defined according to the standard recommendation of the European LeukemiaNet (Dohner H et al, Blood. 2010: 115:453–474).
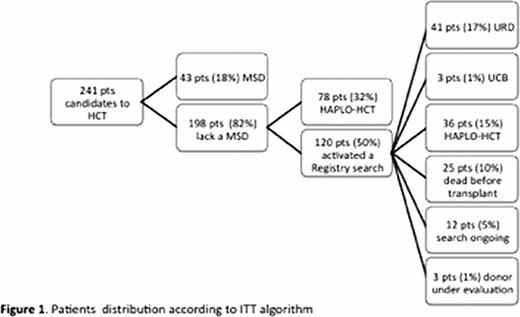
Indication to HCT was given to 241 pts (median age 52y, r17-72, 66 pts over-60y; male 138). HCT was performed in 201/241 pts (median time from diagnosis to HCT 222 days, median time from HCT-indication to HCT 80 days), 24/201 pts received a second HCT due to disease relapse.
Pts distribution according to ITT algorithm is reported in figure 1. In ITT analysis, 83,4% of candidate pts received an HCT.
Characteristic related to pts/disease/transplant are reported in table 1.
Noteworthy, pts in 1st complete remission (CR1) are evenly distributed according to donor source (namely HLA-matched sibling donor – MSD, unrelated donor – URD, haploidentical related donor - haplo-HCT).
The overall survival (OS) analysis for pts transplanted in CR is 71% at 1y and 56% at 3y, for pts in morphologic leukemia free state (MLFS) 32% and 21%, for pts in relapse 23% and 11% (p<0.0001). The relapse incidence (RI) for pts in CR at 1y and 3y is 17% and 21%, for pts in MLFS 43% and 43%, for pts in relapse 35% and 36% (p0.00205). The 1–3y transplant related mortality (TRM) is 16%-28% for CR pts, 31%-44% for MLFS pts, 48%-53% for relapse pts (p<0.0001).
The comparison between pts transplanted in 1st CR versus (vs) 2nd CR shows: 1–3y OS 75%-64% vs 64%-44% (p0.0152), 1–3y RI 9%-12% vs 25%-30% (p0.008), while TRM is superimposable.
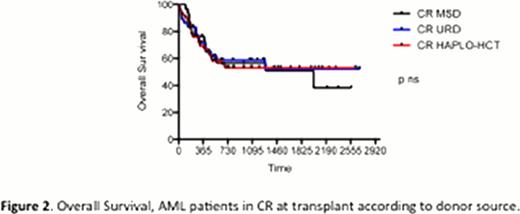
For pts transplanted in CR, the 1–3y OS according to donor source (MSD, URD, haplo-HCT) is 76%-57% vs 68%-59% vs 69%-53% (p ns) – figure 2; the 1–3y TRM is 23%-37% vs 12%-18% vs 16%-28% (p ns); the 1–3y RI is 7%-14% vs 20%-23% vs 20%-22% (p ns).
For pts in 1st CR, the 1–3y OS according to donor source (MSD, URD, haplo-HCT) is 68%-53% vs 86%-73% vs 72%-67% (p ns). TRM and RI are superimposable.
For pts in any CR, the 1–3y OS according to disease characteristics (primary AML vs therapy related AML vs AML with myelodysplasia related changes) is 73%-60% vs 50%-50% vs 59%-46% (p ns).
For pts transplanted in relapse, the 1 OS according to donor source (MSD, URD, haplo-HCT) is 21% vs 33% vs 21% (p ns), TRM and RI are superimposable, long term survivors are present only in haplo-setting (5y OS 10%).
For many pts with high risk AML, HCT from a MSD provides the best chance for long-term survival. However, only approximately 30% of individuals have a MSD. In our experience, the option of HCT for adults with AML is no longer limited to those pts with MSD thanks to the exploitation of an high-committed strategy of donor search for pts in need and of haplo-HCT as alternative donor source. Haplo-HCT offers a concrete option of cure to AML pts: outcome results (OS TRM RI) are superimposable to MSD and URD in any setting, noteworthy in 1st CR and regardless of disease characteristics.
Patients, disease and transplant characteristics.
| Patient related . | n 201 . | |||
|---|---|---|---|---|
| Median Age | 51-y (r 17-72) | |||
| Over 60 y | 53 (26%) | |||
| Male sex | 108 (54%) | |||
| Disease related | n 201 | |||
| Primary AML | 129 (64%) | |||
| Therapy related AML | 15 (8%) | |||
| AML with myelodysplasia-related changes | 57 (28%) | |||
| Transplant related | n 225 | |||
| Donor | MSD | URD | UCB | haplo-HCT |
| n | 45 (20%) | 42 (19%) | 7 (3%) | 131 (58%) |
| Status at transplant | ||||
| - CR1 | 26 (58%) | 24 (57%) | 0 | 26 (20%) |
| - CR2 =>/2 | 4 (9%) | 12 (29%) | 2 (28%) | 24 (18%) |
| - MLFS | 1 (2%) | 3 (7%) | 2 (28%) | 7 (5%) |
| - relapse | 14 (31%) | 3 (7%) | 3 (43%) | 74 (57%) |
| Patient related . | n 201 . | |||
|---|---|---|---|---|
| Median Age | 51-y (r 17-72) | |||
| Over 60 y | 53 (26%) | |||
| Male sex | 108 (54%) | |||
| Disease related | n 201 | |||
| Primary AML | 129 (64%) | |||
| Therapy related AML | 15 (8%) | |||
| AML with myelodysplasia-related changes | 57 (28%) | |||
| Transplant related | n 225 | |||
| Donor | MSD | URD | UCB | haplo-HCT |
| n | 45 (20%) | 42 (19%) | 7 (3%) | 131 (58%) |
| Status at transplant | ||||
| - CR1 | 26 (58%) | 24 (57%) | 0 | 26 (20%) |
| - CR2 =>/2 | 4 (9%) | 12 (29%) | 2 (28%) | 24 (18%) |
| - MLFS | 1 (2%) | 3 (7%) | 2 (28%) | 7 (5%) |
| - relapse | 14 (31%) | 3 (7%) | 3 (43%) | 74 (57%) |
Bordignon:MolMed SpA: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal