Abstract
Abstract 1919
Neutrophil extracellular traps (NETs), originally discovered as a component of innate antimicrobial immunity, are chromatin and granule proteins released from activated neutrophils to form extracellular fibrillar matrices. Recently, NETs have been proven to contribute to inflammation and thrombosis and are elevated during such diseases as systemic lupus erythematosus, sepsis, and thrombotic thrombocytopenic purpura. Following allo-SCT, patients are often prone to infectious and thrombotic episodes, especially those complicated with SCT-associated thrombotic microangiopathy (TMA). However, the relevance of serum NETs to the incidence of TMA after allo-SCT has not been reported. This study aimed to analyze serum NET trends during allo-SCT and define their effects on the risks of TMA.
We retrospectively reviewed the clinical history of patients who underwent allo-SCT in our department between Sept 2007 and Apr 2012. Patients' serum specimens were collected at 3 different times (before conditioning regimen [PRE], on Day0, and Day 28 [4WK]). TMA was diagnosed according to the EBMT criteria (schistocytes increase, thrombocytopenia, LDH elevation, and decrease of hemoglobin and haptoglobin levels). Patients who met these criteria at least once were included in the TMA group. The serum specimens were analyzed using PicoGreen dsDNA Quantitation Kits (Invitrogen). Univariate analyses for the cumulative incidence of TMA were carried out using Gray's methods considering death as a competing risk. Factors associated with at least borderline significance (p < 0.10) were subjected to a multivariate analysis, using Fine-Gray proportional hazards models.
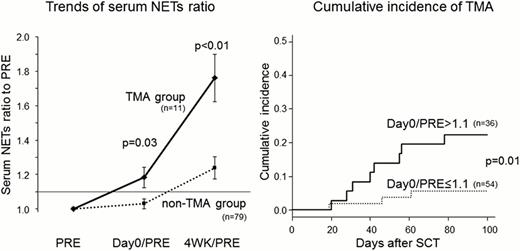
Ninety patients were included (M:F, 50:40), whose age ranged from 17 to 66 years (median, 48.5). The underlying diseases were AML in 34; MDS, 10; ALL, 16; ML, 21; and others, 9 patients. Disease status at SCT was progressive (less than PR) in 36 cases. Donors were related in 20 cases. Myeloablative conditioning (MAC) was performed in 39 cases. Prophylaxis for aGVHD comprised a calcineurin inhibitor (CNI, CyA; 16, FK506; 74) plus MTX (47 cases) or MMF (7 cases). With the median follow-up of 700 days (range, 98–1660), TMA was reported in 11 cases, at a median of 42 days (range, 19–78) after SCT, and the cumulative incidence was 12.2% (95% CI, 6.5–19.9%). The serum NET values of PRE (102.7 ± 4.9 ng/mL, mean ± standard error mean) or Day0 (102.6 ± 4.4) for SCT patients were almost similar to those for healthy donors (107.0 ± 5.2, n = 10). In contrast, the values at 4WK for SCT patients were apparently elevated (123.6 ± 5.9), especially in the TMA group (150.3 ± 13.3). Interestingly, the ratio of Day0 to PRE values (Day0/PRE) and 4WK to PRE (4WK/PRE) were significantly higher in the TMA group, compared with non-TMA group (1.18 ± 0.05 vs 1.03 ± 0.02 in Day0/PRE [p = 0.03], and 1.76 ± 0.13 vs 1.23 ± 0.06 in 4WK/PRE [p < 0.01]). Univariate analysis showed that the incidence of TMA was significantly higher in patients with Day0/PRE > 1.1 (36 cases) than those with a ratio ≤ 1.1 (54 cases) (22.2 vs 5.6%, p = 0.01). Other risk factors of TMA were blood-type minor mismatch (incidence of TMA; 17.2 vs 3.1%), and progressive disease (22.2 vs 5.6%). Non-significant factors included donor source, sex, older age, underlying disease, MAC, TBI, and type of CNI (p > 0.10). Multivariate analysis showed that Day0/PRE > 1.1 was significant (hazard ratio 4.55, p = 0.04). The 1-year OS was significantly lower (31.2 vs 69.8% [p < 0.01]) and TRM was higher (39.0 vs 9.3% [p = 0.03]) in the TMA group than in the non-TMA group. Day0/PRE ratio did not have a significant impact on the incidence of other early complications such as aGVHD (38.9 vs 55.6%) or bacterial infections (55.6 vs 37.0%) in the Day0/PRE > 1.1 and ≤ 1.1 groups.
Higher 4WK/PRE ratios of serum NETs showed the possible contribution of NETs to the pathogenesis of TMA. Elevation of Day0/PRE ratios was shown to significantly increase the incidence of TMA after SCT. Increased amounts of intravascular NETs released from activated neutrophils following conditioning regimens may cause endothelial damage and thrombotic tendencies associated with platelet aggregation, resulting in TMA coupled with other post-transplant factors such as infection, CNI administration, and GVHD. A Day0/PRE serum NET ratio > 1.1 is a risk factor for TMA, and prophylactic strategies should be attempted to improve the outcomes of allo-SCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal