Abstract
Abstract 1851
Bendamustine, an agent sharing properties of alkylators and purine analogous, showed a strong efficacy and safe toxicity profile in relapsed multiple myeloma (MM) patients (pts), with a maximally tolerated dose (MTD) ranging from 100 mg/m2/die day 1 and 2 as single agent to 60 mg/m2/die in association with thalidomide. In a pooled analysis of two large phase 3 trials Lenalidomide, an analogous of thalidomide with strong activities in MM, significantly improved overall response rate and progression-free survival. Since the role of Lenalidomide in the treatment of naïve and relapsed/refractory pts has been well established, the current research is focused on the combination of Lenalidomide with chemotherapy to further improve patient outcome.
This multicenter phase I/II trial was designed to investigate the combination of Bendamustine, Lenalidomide, and Dexamethasone (BdL) in repeating 4-week cycles as treatment for relapsed MM. Pts over 18 years with measurable stage II or III MM who relapsed after 1 to 3 previous lines of therapy, including bone marrow transplantation were considered eligible. Prior Lenalidomide and Bortezomib were allowed.
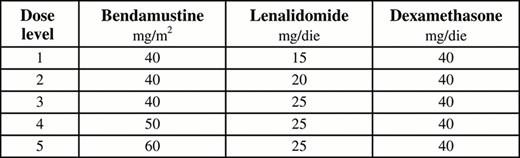
The phase I study was conducted using a 3+3 cohort design beginning at a dose level 0 of intravenous Bendamustine 40 mg/m2/die days 1 and 2, oral Lenalidomide 10 mg/die days 1–21 and oral Dexamethasone 40 mg/die days 1, 8, 15, and 22 (28-day cycle).
The dose of Bendamustine and Lenalidomide (from 0 to 5) were increased from one cohort to the next, in a 3+3 dose escalation scheme to reach the MTD (Table 1).
The MTD of Bendamustine and Lenalidomide were evaluated during the first treatment course (cycle 1). Enrollment at each subsequent dose level was permitted only if the first 3 patients at the previous level received 1 cycle with an acceptable dose-limiting toxicity (DLT).
DLTs were defined as any adverse event (AE) possibly related to the study drug ≥grade 3 CTC. If 1 of the 3 subjects experienced DLT during the first cycle, 3 more subjects were to be recruited and treated at the same dose level of Bendamustine and Lenalidomide.
Treatment was given until plateau of best response according to the International Myeloma Working Group uniform response criteria for a maximum of 6 cycles.
Herein, we present the results from phase I of the study which established MTD. Fifteen pts with a median age of 69 years (range 49 to 88) were enrolled between October 2011 and February 2012. The number of prior therapies was at maximum 3 as per protocol: Lenalidomide (27% of pts), thalidomide (33% of pts), Bortezomib (67% of pts) and 13% of the pts had a prior autologous stem cell transplant. Because 3 DTL were observed in Phase I, the MTD was set at 40 mg/m2/die for Bendamustine and 10 mg/die for Lenalidomide. DLTs at dose level 1 included: 1 grade 4 cutaneous rash; at dose level 2: 1 grade 4 thrombocytopenia and 1 grade 3 bronchopneumonia with renal dysfunction (Table 2).
Summary of all treatment-related adverse events observed in 15 patients.
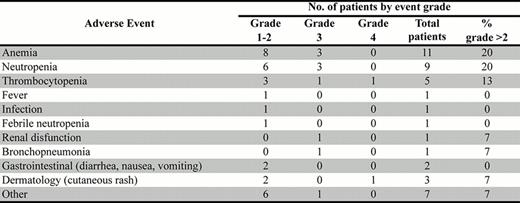
Among the 15 patients with evaluable data, the grade 3 or 4 AEs observed in ≥10% of patients included neutropenia (20%), thrombocytopenia (13%) and anemia (20%). Two patients died of treatment-related complications: 1 for hematological toxicity and CNS hemorrhage, and 1 for cardiac ischemia.
Fifteen patients received at least 2 cycles and were included in the response assessment. The overall response rate was 40% with 1 case achieving complete response and 1 a very good partial response.
Until now 7 pts entered the phase II part of the trial.
In pretreated patients with relapsed MM, MTD was determined to be Bendamustine 40 mg/m2/die on days 1 and 2, and Lenalidomide 10 mg/m2/die on days 1–21, plus Dexametasone 40 mg/die on days 1, 8, 15, and 22. This BdL schedule was relatively tolerated and showed promising efficacy. Based on the mainly myelosuppressive properties, concomitant treatment with growth factors are recommended for all patients. The toxicity profile of BdL scheme resulted in an acceptable treatment-related toxicity and mortality and induced a good quality responses in a pretreated population of MM pts.
No relevant conflicts of interest to declare.
This research was supported in part by the Associazione Angela Serra per la ricerca sul cancro.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal