Abstract
Abstract 1677
BCR-ABL1 kinase domain (KD) point mutation causes resistance to tyrosine kinase inhibitors (TKI) in CML patients through impaired binding of TKI to the target site. One of the characteristics of patients with BCR-ABL1 kinase domain point mutations is the fact that some patients have multiple mutations. However there have not been many studies showing that data about clinical relevance or dynamics of multiple mutation during CML treatment.
Since 2002, 414 CML patients were screened for mutation analysis due to sign of resistance to TKI including imatinib, nilotinib, dasatinib, bosutinib, radotinib or ponatinib at Seoul St Mary's Hospital using direct sequencing and ASO-PCR. Among them, 31 patients showed multiple mutations. We analyzed serial samples from the 31 patients using subcloning and sequencing to investigate whether the multiple mutations are on same clone (defined as compound clone), separated clones (defined as multiple clone) or co-existent clones (defined as mixed clone) and characterize its clinical relevance and dynamics.
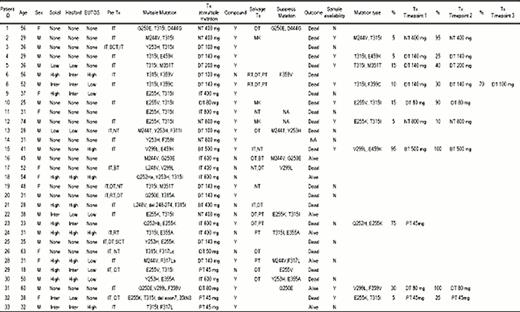
Status of the patients with multiple mutations is shown in Table 1. In order to investigate whether the multiple mutations are on same clone or on separated clone, we cloned serial samples from the 31 patients. Cloning of cDNA region corresponding to BCR-ABL1 KD into plasmid was performed and followed by transformation into competent cells, colony formation, plasmid preparation of 20 colonies from each sample, and then direct sequencing.
Multiple mutations of 65% patients (20 out of 31) existed compound mutation which means the individual mutant types are located on the same BCR-ABL1 molecule. In addition of major mutation types which were detectable in direct sequencing analysis, all the patients showed to have minor types of mutations which were found only through BCR-ABL1 KD cloning and subsequent colony sequencing. To make sure that this minor mutation types were not caused by sequencing error, we also analyzed of 3 patients who showed TKI resistance, but had no BCR-ABL1 mutation. In addition, samples from 3 normal persons were analyzed with the same method. The frequency of appearance of the minor types of point mutation was reduced in the patient group who showed TKI resistance, but had no BCR-ABL1 mutation, and then dramatically decreased in the normal person group, indicating that BCR-ABL1 gene in patients with point mutation are relatively unstable.
Among 20 patients with compound mutation, 9 patients were available for serial timepoint samples under same TKI therapy. In all nine patients (100%), portion of compound clone was increased as treatment went on. With a median follow-up 53.3 months (range, 0–113.2 months), of 31 patients with multiple mutation, 7 patients remained alive; 4 of 11 (36%) in the multiple clone group vs 3 of 20 (15%) in the mixed clone group (P = 0.066).
Analysis of serial samples from a same patient provided evidence of dynamic change of portion of compound mutation. In most case, portion of the clone containing compound mutation was increased as treatment went on, indicating the clone harboring compound mutation can take survival advantage over TKI treatment in comparison of the clone containing individual type of mutation. In addition, some patients showed change in individual mutation type comprising multiple mutations as treatment went on. Patients with compound clone showed poor outcomes compared with multiple clone group in our cohort, further investigation on a large patient cohort will be needed. Updated data with longer follow-up duration will be presented in the meeting.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal