Abstract
Abstract 1619
Double-hit lymphomas (DHL) harboring rearrangements or additional copies of MYC and BCL2 or less commonly BCL6 have been associated with a poor prognosis, but data remains limited. We conducted a retrospective analysis of DHLs to evaluate for factors associated with an improved prognosis.
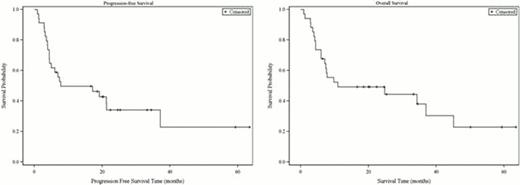
We identified DHL cases diagnosed 2004–2011. Cases were included if they had rearrangements or extra copies of MYC as well as BCL2 or BCL6, or both. Overall survival (OS) was defined as the time from biopsy to death. Progression-free survival (PFS) was defined as time from biopsy to progression or death without progression. OS and PFS curves were obtained using the Kaplan-Meier method with 90% confidence intervals calculated using Greenwood's formula. Univariate analysis for risk factors was conducted with the log-rank test using a two-sided significance level of 0.05. Stepwise multivariable Cox regression analyses of PFS and OS were utilized to identify significant prognostic factors.
Thirty-four DHL patients were included in the analysis. Twenty-eight patients (82%) had rearrangements of both MYC and BCL2, one of whom also had a BCL6 translocation. Two patients had rearrangements of MYC and BCL6. One patient each had rearrangement of MYC with 8 copies of BCL2, rearrangement of BCL2 with 3 copies of MYC, rearrangement of BCL2 with 4 copies of MYC, and rearrangement of BCL6 with 4 copies of MYC. Based on the WHO classification, 35% had DLBCL morphology, while 65% had B-cell lymphoma unclassifiable with intermediate features between DLBCL and BL (BCLU). Median Ki67 was 90% (range 25–100%). The median age was 63 (range 32–86 years), and gender was evenly divided. Prior follicular lymphoma was present in 10 patients (29%). Twenty-nine patients (85%) had advanced stage disease, with 27 (79%) presenting at stage IV and 2 at stage III. Five patients (15%) had limited-stage disease. Extranodal disease was present in 26 (77%), including 6 patients with CNS disease, 9 with leukemic disease, and 15 with marrow disease. Eighteen patients (53%) had 2 or more extranodal sites involved at diagnosis. Performance status was 0–1 in the majority of patients (88%). LDH was elevated in 30 patients (88%). The mean LDH was 1388 (range 151 – 10840). The IPI score was 0–1 in 15%, 2–3 in 35% and 4–5 in 50%.
Fifteen (44%) patients were treated with R-CHOP, 6 (18%) with R-CODOX-M/IVAC, 12 (35%) with R-EPOCH, and 1 patient with best supportive care. Two patients underwent consolidative SCT in first remission following R-EPOCH; 1 patient underwent auto SCT, another patient underwent auto SCT followed by reduced-intensity allo SCT on a clinical trial. Complete response were achieved in 22 (64%), partial response in 2 (6%), and progressive disease in 10 (29%). At a median of 25 months, 13 patients (38%) remain alive and free from progression. The median PFS is 8 months (90% CI [5, 21]) and the median OS is 11 months (90% CI [7–37]). Univariate analysis for PFS identified adverse risk factors of elevated LDH, IPI score 4–5, extranodal disease, marrow involvement, and leukemic phase. Univariate analysis for OS identified adverse risk factors to be BCLU morphology, elevated LDH, IPI score 4–5, extranodal disease, and leukemic phase. For both PFS and OS, univariate analysis demonstrated a more favorable outcome in patients with DLBCL morphology, and for those treated with R-EPOCH. Median PFS and OS for R-EPOCH patients were 21 and 34 months, respectively, compared to 6 and 8 months for R-CHOP, and 6 and 7 months for R-CODOX-M/IVAC. Multivariable analysis for PFS identified presence of extranodal disease (HR 19, 90%CI[3.3–112]) and BCLU morphology (HR 5.2, 90%CI[1.9–14]) as adverse predictors of outcome. Multivariable analysis for OS identified leukemic disease as an adverse risk factor (HR 6.6, 90%CI[2.4–18]) and R-EPOCH therapy as a protective factor (HR 0.3, 90%CI[0.1–0.9]).
DHLs are highly aggressive lymphomas with a poor overall prognosis. A subset, however, will present with more favorable characteristics predicting a higher rate of cure, including DLBCL morphology, normal LDH, absence of extranodal disease and IPI score of 0–2. R-EPOCH may perform better than other regimens, though this requires prospective validation in larger series.
Abramson:Genentech: Consultancy. Hochberg:Genentech: Consultancy; Biogen-Idec: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal