Abstract
Abstract 1596
The IPI, which takes into consideration both host and tumor factors, is the standard method used to stratify aNHL into different risk categories. The IPI was derived in the pre-rituximab era and confirmed as valid in the Rituximab (R) era. The major mechanism of action of R appears to be through the host's immune system. Host factors related to the immune status have been recently recognized as significant in predicting outcome. The ALC, AMC, and ALC/AMC ratio were identified by Wilcox et al. as having an impact on both progression free survival (PFS) and overall survival (OS) (Leukemia 2011;25:1502-09). In order to confirm these findings in a different population of aNHLs we have studied 402 patients with aNHL treated in the R era at 5 centers: 1 in Puerto Rico, 4 in Spain (1 Barcelona, 2 Madrid, 1 Valencia).
402 patients diagnosed between December 2000 and April 2011 with aNHL were included. ALC and AMC were obtained from pretreatment CBC. All patients received anthracycline and R based chemotherapy. ALC was divided in quartiles (Q): 1st Q ALC ranged between 277 and 950, 2nd Q ALC 951–1352, 3rd Q ALC 1353–1870, and the 4th Q ALC 1871– 5400. The lower Q ALC of 950 and the median of 1353, as well as the lower Q AMC of 366 and the median AMC of 504 were assessed as cutoffs to divide patients into groups with low or high ALC and AMC.
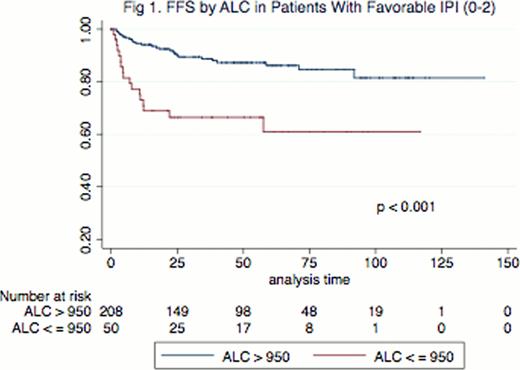
Median age was 64 (17–92) and 55% were females. Median follow up was 50 months. FFS and OS at 4 years were 73% and 79% respectively. FFS was superior for patients with an ALC >950 vs <=950 (78% vs 57% respectively, p<0.0001) as well as OS (83% vs 67%, P=0.0008). A progressive and gradual improvement in 4 yr FFS was observed as the ALC increased in the 4 quartiles: 57% for the lower quartile, 73% for the 2nd quartile, 74% for the 3rd quartile and 84% for the 4th quartile (p=0.0008). However, the AMC was not predictive of FFS in this cohort (72% vs 73% for AMC >=366 vs <366 respectively, p=0.8 and 71% vs 74% for AMC >=504 and <504, respectively, p=0.8). 4 yr FFS and OS was superior for patients with a favorable IPI of 0–2 (83% and 88%) as compared with unfavorable IPI (>2) whose 4 yr FFS and OS were 53% and 65% respectively (p<0.0001). In order to evaluate the independent contribution of ALC to IPI we first focused on those with low IPI, and found that 4 yr FFS for favorable IPI cases with ALC >950 vs <=950 was 87% vs 67%, (p <0.001, Fig 1). We then looked at those with unfavorable IPI and found that those with ALC <=950 had 4 yr FFS of 48%, but using the 4th ALC quartile as cutoff, patients with an ALC over 1870 had a FFS of 70%. This finding however, was not statistically significant (p=0.3). There was no difference in FFS or OS by gender but male patients with a lower ALC had a significantly worse FFS and OS than those with a higher ALC (FFS 77% vs 50%, p <0.001 and OS 85% vs 60% p=0.002) while this difference was not seen in females, where FFS and OS by ALC were not statistically significant (78% vs 66%, p=0.09 for FFS and for OS 83% vs 74%, p=0.15). On multivariate analysis the IPI and ALC remained as independent prognostic factors for FFS (p<0.001, HR 3.04 and p=0.01 HR 1.68, respectively) and OS (p<0.001, HR 2.61 and p=0.02 HR 1.68, respectively).
We have confirmed that the ALC is an independent prognostic factor for FFS in aNHL. It can identify patients with an inferior outcome despite having a favorable IPI and its effect seems to be more striking in males than in females. In contrast to Wilcox's findings, the AMC and ALC/AMC ratio was not an important predictor of FFS and OS in our cohort. Improved FFS in patients with higher ALC suggests that the immune system plays an important role inthe outcome of patients treated with R-chemo.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal