Abstract
Abstract 1590
Skeletal involvement (SI) is observed at low prevalence in patients with diffuse large B-cell lymphoma (DLBCL). Although extranodal lymphoma sites are generally regarded a risk factor, as reflected in the international prognostic index (IPI), there is limited data on prognostic factors further differentiating outcome in patients with DLBCL and SI due to the rareness of this particular entity. Whether there is a need for intensification of chemotherapy or combination with radiotherapy in all of these patients is a matter of debate.
Medical charts of the Department of Hematology and Oncology from the University of Heidelberg Hospital were retrospectively reviewed in regard to patient characteristics, treatment and outcome. Progression-free survival (PFS) and overall survival (OS) were estimated using the Kaplan-Meier method. The impact on PFS and OS of variables was evaluated by univariate log-rank tests.
A total of 812 patients with DLBCL were treated between January 2000 and December 2011. Of these, 75 patients (9.2%) were found to have presented with SI at initial diagnosis. Median age of patients with DLBCL and SI was 53.6 years [range 16–83]; 51 patients were male. 2 year (y) PFS was 76% and 2y OS was 81%. According to IPI, 18 (24%) were low risk (IPI 0–1), 35 (47%) intermediate risk (IPI 2–3) and 16 (21%) high risk (IPI 4–5); 6 patients had a missing IPI score. Of the five IPI components, only Ann Arbor stage III-IV was significantly associated with both reduced PFS and OS (p < 0.001). In contrast, neither ECOG > 1 nor extranodal sites > 1 were significantly associated with PFS or OS. We additionally analysed the impact of a higher number of extranodal sites, multilocular SI as well as of elevated serum calcium and serum AP levels (both thought to be indicative of increased bone metabolism) on patients' survival. We found that more than 3 extranodal sites as well as hypercalcemia were significantly associated with both reduced PFS and OS (p < 0.001 and p < 0.01, resp.), whereas elevated serum AP and multilocular SI had no impact.
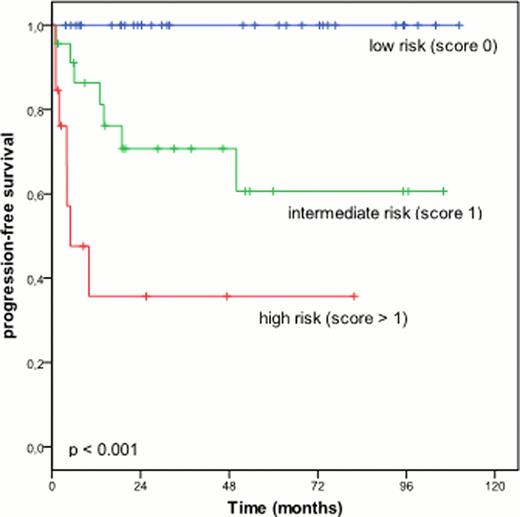
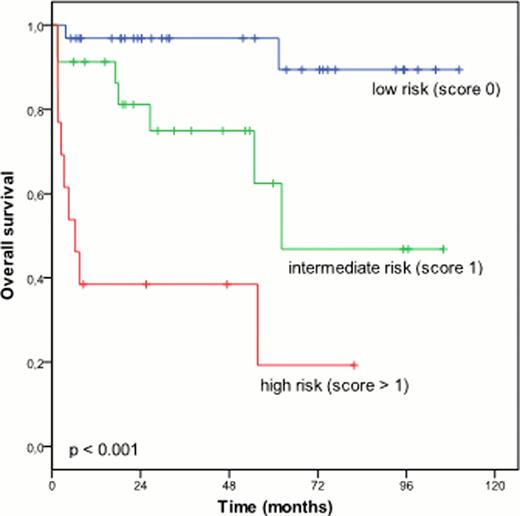
In a next step, we developed a novel prognostic score taking into account the presence of hypercalcemia, extranodal sites > 3 and Ann Arbor stage III-IV (one point each). According to this score, 32 (43%) were low risk (0 points), 23 (31%) intermediate risk (1 point) and 13 (17%) high risk (> 1 point); 7 patients had no evaluable score due to missing variable. 2y PFS for score 0, 1, and > 1 was 100%, 71% and 36%, resp.; 2y OS was 97%, 81% and 39%, resp. (figure 1). No significant difference in regard to first-line treatment modalities was noticeable between different score groups. Patients in the low risk group (score 0) had an excellent outcome independently of addition of rituximab, escalation of standard CHOP chemotherapy to a more aggressive regimen or additional radiotherapy. In contrast, patients with score > 0 showed improved outcome with the addition of rituximab (2y PFS 61% vs 33%, p < 0.01; 2y OS 68% vs 33%, p = 0.06) as well as a trend to benefit from a more aggressive chemotherapy regimen than CHOP (2y PFS 73% vs 50%, p = 0.17; 2y OS 82% vs 56%, p = 0.14). Radiotherapy did not seem to have a significant impact.
Patients with DLBCL and SI are a very heterogeneous population. A novel prognostic score comprising hypercalcemia, extranodal sites > 3 and Ann Arbor stage III-IV allows the identification of a large proportion of low risk patients with excellent outcome independently of treatment modalities. In contrast, patients with a higher risk score seem to benefit from the addition of rituximab as well as from a more aggressive chemotherapy regimen than standard CHOP.
PFS and OS according to new prognostic score
PFS and OS according to new prognostic score
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal