Abstract
Abstract 155
Bendamustine is a unique alkylating agent, active as monotherapy and in combination with rituximab for relapsed and refractory indolent non-Hodgkin's lymphoma (NHL). This study compared efficacy and safety of bendamustine-rituximab (BR) with standard treatment regimens of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) and rituximab, cyclophosphamide, vincristine, and prednisone (R-CVP) in first-line treatment of patients with indolent NHL or mantle cell lymphoma (MCL). The primary objective was to determine whether the complete response rate for BR was noninferior to R-CHOP/R-CVP (presented separately). The present analysis reports results for quality of life (QOL) as measured by the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire (QLQ-C30).
Previously untreated patients with indolent NHL or MCL were randomized to receive BR (bendamustine 90 mg/m2/day on days 1 and 2; rituximab 375 mg/m2 on day 1 of each 28-day cycle) or R-CHOP/R-CVP (rituximab 375 mg/m2 and vincristine 1.4 mg/m2 (up to maximum 2 mg) on day 1 and prednisone at 100 mg on days 1–5 (of a 21-day cycle), plus either [1] cyclophosphamide 750 mg/m2 and doxorubicin 50 mg/m2 on day 1 or [2] cyclophosphamide 750 mg/m2 or 1000 mg/m2(investigator choice) on day 1. QLQ-C30 was administered at screening (baseline); after cycles 1, 3, 6, 8; and at the end-of-treatment visit. Linear transformation to standardize raw scores was performed.
The QLQ-C30 is composed of 5 multi-item functional scales, 1 global health status (GHS)/QOL scale, 3 symptom scales, and 6 single-item measures; all scores could range from 0 to 100. Rising scores for functional scales and GHS/QOL indicate improvement. Rising scores for symptom scales/single items indicate worsening. GHS/QOL score change at last QLQ-C30 administration postbaseline was interpreted using analysis of covariance. Data from the last observation (end-of-treatment visit) were analyzed.
The 447 enrolled patients were randomly assigned to 1 of the 2 treatments; 224 to BR (NHL n=187, MCL n=36, missing n=1) and 223 to R-CHOP/R-CVP (NHL n=184, MCL n=38, missing n=1). Treatment groups were well matched for demographic and clinical characteristics.
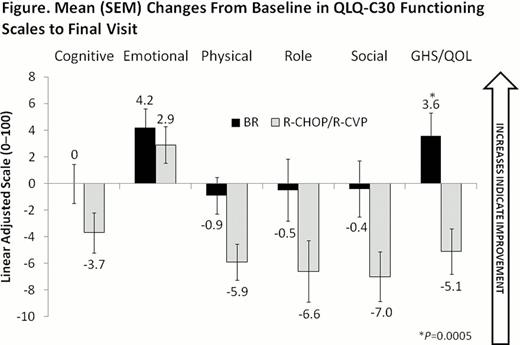
Among all randomized patients, mean change in GHS/QOL score from baseline to final visit was significantly higher (indicating relative improvement) for patients treated with BR than those treated with R-CHOP/R-CVP (3.6 vs −5.1 respectively, P=0.0005). For patients with indolent NHL, mean change in GHS/QOL score by final visit was significantly higher in patients treated with BR than those receiving R-CHOP/R-CVP (2.1 vs −6.3, respectively, P=0.0021); in patients with MCL, mean change in GHS/QOL score was numerically higher in the BR group, but the difference was not statistically significant (10.9 vs 1.6, P=0.0654).
All randomized patients receiving BR showed greater improvement in QLQ-C30 Emotional Functioning (from baseline to final visit), compared with patients receiving R-CHOP/R-CVP. Mean change from baseline scores (± SEM) for QLQ-C30 for Cognitive, Physical, Role, and Social Functioning scales of the QLQ-C30 decreased (signifying deteriorating effect) in both treatment groups, with patients treated with BR deteriorating less than patients treated with R-CHOP/R-CVP (Figure). For symptom scales/item measures, patients treated with BR showed larger reductions in mean scores from elevated baseline levels (signifying greater improvement), compared with R-CHOP/R-CVP for Appetite Loss (−2.9 for BR vs −1.1 for R-CHOP/R-CVP), Pain (−5.6 vs −1.7), and Constipation (−0.7 vs 1.8). For symptom scales/item measures of Dyspnea, Fatigue, and Financial Difficulties, both treatments showed deteriorating effects, with BR showing less than R-CHOP/R-CVP: Dyspnea (0.8 vs 4.8), Fatigue (0.5 vs 7.2), and Financial Difficulties (0.9 vs 1.3). Patients receiving R-CHOP/R-CVP had larger reductions in mean scores for Insomnia (−2.1 for BR vs −6.7 for R-CHOP/R-CVP), Diarrhea (0.5 vs −1.3), and Nausea and Vomiting (1.8 vs 0.9).
In this study, BR significantly improved GHS/QOL, compared with R-CHOP/R-CVP treatment, in previously untreated patients with indolent NHL or MCL. In addition, BR provided improved patient QOL scores for most aspects of functioning and symptoms, as measured by the QLQ-C30.
Support: Teva Pharmaceutical Industries Ltd.
Burke:Spectrum Pharmaceuticals: Consultancy. Off Label Use: Bendamustine is FDA-approved for adults with chronic lymphocytic leukemia or indolent B-cell non-Hodgkin's lymphoma that has progressed during or within six months of treatment with rituximab or a rituximab-containing regimen. Van der Jagt:Celgene: Consultancy, Research Funding, Sponsorship Other; Novartis: Consultancy, Research Funding, Sponsorship, Sponsorship Other; Roche: Consultancy, Sponsorship, Sponsorship Other; Teva: Consultancy, Research Funding; Incyte: Research Funding; Xanthus: Research Funding; Bristol-Myers Squibb: Consultancy. Kahl:Genentech: Membership on an entity's Board of Directors or advisory committees, Research Funding; Roche: Membership on an entity's Board of Directors or advisory committees, Research Funding; Teva: Membership on an entity's Board of Directors or advisory committees. MacDonald:Lundbeck: Membership on an entity's Board of Directors or advisory committees; Roche: Membership on an entity's Board of Directors or advisory committees, Research Funding. White:Teva Pharmaceutical Industries Ltd.: Employment. Munteanu:Teva Pharmaceutical Industries Ltd.: Employment. Clementi:Teva Pharmaceutical Industries Ltd.: Employment. Chen:Teva Pharmaceutical Industries Ltd.: Employment. Flinn:Teva: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal