Abstract
Abstract 1066
Group B Streptococcus (GBS), or Streptococcus agalactiae, is one of the most common cause of life-threatening sepsis in human newborns and immunosuppressed population. Patients suffering from sepsis often display low platelet counts characterized by thrombocytopenia as a result of platelet activation. Platelets, best known for their maintenance of hemostasis, have retained features of archetypal inflammatory cells corresponding to multiple roles in antimicrobial host defense. Nine members of the Toll-like receptors (TLRs) have been reported in human platelets, and TLRs in platelets play a fundamental role in both the initiation and propagation of the inflammatory response to microbial infection. We reported previously that LPS induces platelets activation and enhances platelets to release tumor necrosis factor-α by TLR 4. Since few confirm that platelets were activated by TLRs in directly binding to bacteria, the mechanism of activation of platelets in the interaction with pathogens remains unclear. Our research aimed to verify the hypothesis that the platelets selectively bind or adhere strains of GBS and aggregate, and to investigate the mechanism through which platelets become activated in sepsis upon binding to GBS and platelet TLR 2 involves in the process.
Six strains of GBS were separated from septic patients. We determined GBS inducible platelet reactivity by using light transmission aggregometry, platelet bacterial adhesion assay, FCM and scanning electron microscopy. TLR2 expression was determined by RT-PCR and western blot assay.
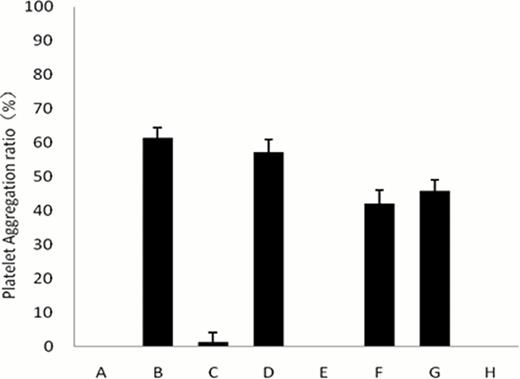
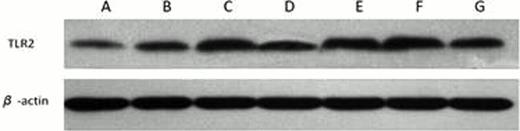
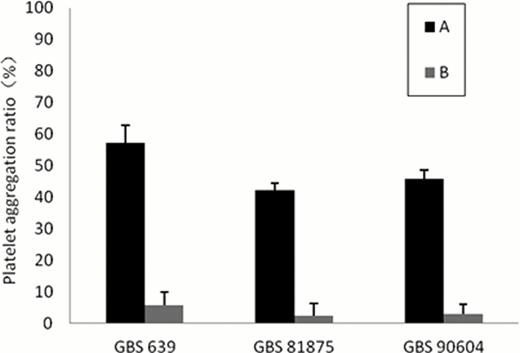
After incubating platelets with strains of GBS separately, only three strains of GBS could induce platelets activation (platelets aggregation, adhesion and upgrated the expression of CD62P on platelet, Figure 1), meanwhile the activating ability and lag time were strain-dependent. Strains of GBS that were able to induce platelets activation also upregulated the expression of platelets TLR2 (in levels of RT-PCR and protein, Figure 2). However incubated with TLR 2 antibody, platelets no longer aggregated by the stimulation of GBS (Figure 3), suggesting TLR2 was involved in GBS induced platelets activation
Different strains of GBS induced platelets aggregation in vitro. Plasma incubated with PBS as negative control (A). Plasma incubated with ADP as positive control (B). Plasma incubated with GBS 255 (C), GBS 639 (D), GBS 945 (E), GBS 81875 (F), GBS 90604 (G) and GBS 93555 (H).
Different strains of GBS induced platelets aggregation in vitro. Plasma incubated with PBS as negative control (A). Plasma incubated with ADP as positive control (B). Plasma incubated with GBS 255 (C), GBS 639 (D), GBS 945 (E), GBS 81875 (F), GBS 90604 (G) and GBS 93555 (H).
Different strains of GBS upgrated TLR2 expression in platelet. A)Plasma incubated with PBS as negative control. Plasma incubated with B) GBS 255, C) GBS 639, D) GBS 945, E) GBS 81875, F) GBS 90604, G) GBS 93555.
Different strains of GBS upgrated TLR2 expression in platelet. A)Plasma incubated with PBS as negative control. Plasma incubated with B) GBS 255, C) GBS 639, D) GBS 945, E) GBS 81875, F) GBS 90604, G) GBS 93555.
Different strains of GBS induced platelets aggregation, A) before incubated with TLR2 MAb, B) after incubated with TLR2 MAb.
Different strains of GBS induced platelets aggregation, A) before incubated with TLR2 MAb, B) after incubated with TLR2 MAb.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal