Abstract 839 FN2
FN2
Many patients who require allogeneic hematopoietic stem cell transplantation (allo-HSCT) lack a human leukocyte antigen (HLA)-matched donor. Recently, we developed a new strategy named GIAC protocol for HLA-mismatched/haploidentical transplantation from family donors that combines granulocyte-colony stimulating factor (G-CSF) primed bone marrow (G-BM) and peripheral blood stem cells (PBSC) without in vitro T-cell depletion (TCD). For the past nine years, promising results for HLA-mismatched allo-HSCT without in vitro TCD have been achieved at our institute using this protocol. From May 2002 to December 2010, 820 patients, including 206 in high-risk group, underwent transplantation from haploidentical family donors. Eight-hundred and eleven patients (99%) achieved sustained, full donor chimerism. The incidence of grade 2–4 acute graft-versus-host disease (GVHD) was 42.9%, and that of grades 3 and 4 was 14.0% which was not associated with the extent of HLA disparity.Close modal
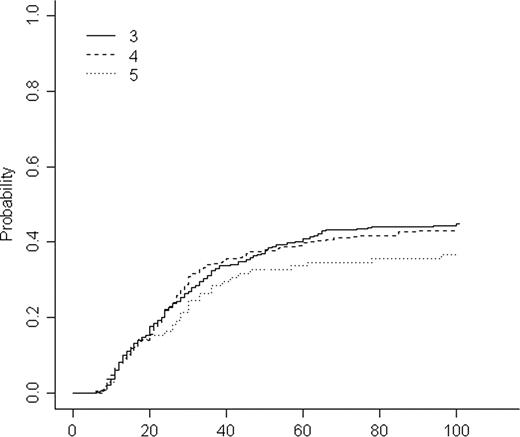
Figure 1
Cumulative incidence of acute GVHD grade 2–4 according to HLA disparity.
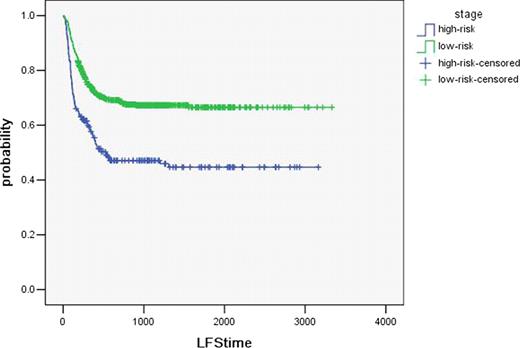
Figure 2
Probability of LFS after haploidentical HSCT according to disease stage (p =.001).
Figure 2
Probability of LFS after haploidentical HSCT according to disease stage (p =.001).
Disclosures:
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
© 2011 by The American Society of Hematology
2011

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal