Abstract
Abstract 589 FN2
FN2
Intensified chemotherapy with eight cycles of BEACOPPescalated in advanced stage Hodgkin lymphoma (HL) is highly effective but also associated with relevant treatment related toxicity. In addition, the need for radiotherapy in this setting is unclear. To reduce toxicity without losing efficacy the German Hodgkin Study Group thus conducted the prospective randomized clinical HD15 trial investigating two less intensive chemotherapy variants, followed by positron emission tomography (PET) guided radiotherapy.
Between January 2003 and April 2008, 2182 patients with newly diagnosed, histology-proven HL aged 18–60 years were included. Patients in Ann-Arbor stage IIB with large mediastinal mass or extranodal lesions, or those in stage III or IV were randomly assigned to receive either eight cycles of BEACOPPescalated (8Besc), six cycles of BEACOPPescalated (6Besc), or eight cycles of BEACOPP14 (8B14). After completion of chemotherapy, patients in partial response (PR) with a persistent mass measuring 2.5 cm or more were assessed by PET. Only patients who were positive on centrally-reviewed PET scan received additional radiotherapy (RT) with 30Gy. The study was designed to show non-inferiority for the primary endpoint, freedom from treatment failure (FFTF). Other endpoints included overall survival, tumor response, side effects of treatment and progression-free survival (PFS) after PET.
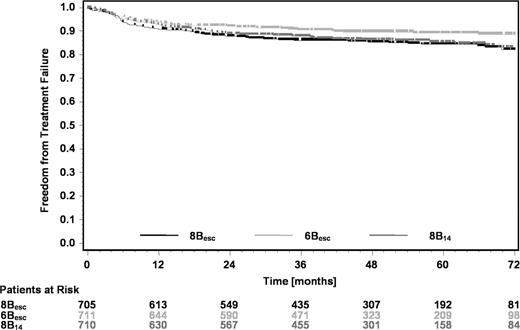
The full analysis set comprised 2126 patients, 705 with 8Besc, 711 with 6Besc and 710 with 8B14. Baseline characteristics were balanced between groups with a median age of 33 years and 334 patients (15.7%) in stage II disease. 682 patients (32.1%) had an International Prognostic Score (IPS) of 0–1, 1115 (52.4%) of 2–3, and 329 (15.5%) of 4–7. Hematological toxicities occurred in 92.4% (8Besc), 91.7% (6Besc), and 79.7% (8B14) of cases. After a median follow-up of 48 months, there were 53 deaths (7.5%) in the 8Besc group, 33 (4.6%) in the 6Besc group and 37 (5.2%) in the 8B14 group. The higher number of deaths in the 8Besc group mainly resulted from acute toxicity of chemotherapy (15 vs. 6 vs. 6) and secondary neoplasms (13 vs. 5 vs. 8). There were 72 secondary cancers including 29 secondary acute myeloid leukemias and myelodysplastic syndroms, 19 (2.7%) after 8Besc, 2 (0.3%) after 6Besc and 8 (1.1%) after 8B14. Complete response (CR) was achieved in 90.1% of patients after 8Besc, in 94.2% after 6Besc and in 92.4% after 8B14 (p=0.01). FFTF at 5 years was 84.4% in the 8Besc group, 89.3% in the 6Besc group (97.5% confidence interval (CI) for difference 0.5% to 9.3%), and 85.4% in the 8B14 group (97.5 CI −3.7% to 5.8%), respectively (see figure). Accounting for planned interim analyses, both 97.5 repeated CIs for the hazard ratio excluded the non-inferiority margin of 1.51 (8Besc vs. 6Besc, 0.44 to 1.02; 8Besc vs. 8B14, 0.62 to 1.36). Overall survival at five years was 91.9%, 95.3%, and 94.5%, and was also better with 6Besc compared to 8Besc (97.5% CI 0.2% to 6.5%). PFS results were similar to FFTF. Per-protocol and subgroup analyses supported the primary analysis. PET scans performed after chemotherapy were centrally reviewed in 822 patients of whom 739 were in PR with residual mass ≥ 2.5 cm having no other exclusion criteria. 548 patients were PET-negative (74.2%) and 191 were PET-positive (25.8%). Importantly, PFS was comparable between patients in CR or those in PET-negative PR after chemotherapy with 4-year PFS rates of 92.6% and 92.1%, respectively. Only 11% of all patients in HD15 received additional RT as compared to 71% in the prior HD9 study.
Six cycles of BEACOPPescalated followed by PET-guided RT are more effective and less toxic compared to 8 cycles in patients with advanced stage HL. In particular, critical toxicities observed with 8 cycles where reduced with 6 cycles of BEACOPPescalated. PET performed after chemotherapy can guide the need of additional RT in this setting and reduces the number of patients requiring RT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal