Abstract
MDS is a disease of predominantly elderly patients with a median age of >70 years. At present there is a lack of data on MDS patient management in Germany. The following analysis offers a comprehensive insight into diagnosis, prognosis and management of MDS in German clinical practice. First results in 2009 showed that age was a key decision driver for MDS management, particularly with regards to cytogenetic testing, IPSS evaluation and choices of active treatment. The aim of a 2010 update was to monitor changes in management of MDS patients, especially in patients >75 years of age.
The patient sample was defined based on a structural analysis taking into account the distribution of treatment prevalence by institutional type as well as the regional population density. 886 centers involved in MDS management including university hospitals (UH), community hospitals (CH) and office-based hematologists (OBH) were contacted. 94 centers provided information on their respective patient numbers during the third quarter of 2010, with 1,611 patients corresponding to 12% of the estimated national prevalence. The distribution of patients by institution was 10% UH, 55% CH, and 35% OBH. In order to adequately represent UH and to avoid bias due to a too small sample size, the proportion of patients treated in UH was adjusted to 33% in our sample. The adjusted sample consisted of 46 centres (12 UH, 15 CH and 19 OBH) which documented 365 patients. Patient samples in 2010 and 2009 were comparable. Consistent with 2009, patients with a treatment decision (diagnosis, start, change or termination of therapy) in the third-fourth quarter were included in this analysis.
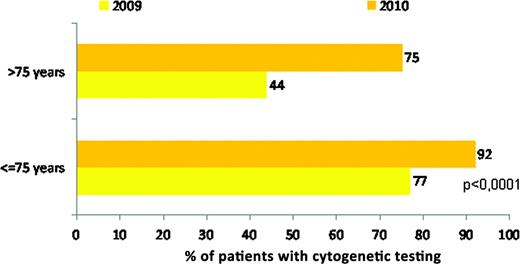
Compared to 2009, cytogenetic testing at first diagnosis substantially increased from 67% to 86% in 2010. The biggest change was observed in patients >75 years with an absolute increase of 31%, reaching 75% in 2010 (fig. 1). Despite this change, a significant difference still remains in the level of cytogenetic testing between patients '75 and >75 years (92% vs. 75%, p<0,0001) and a higher use in UH compared to OBH (96% vs. 84%, p<0,0001). Overall, prognostic IPSS assessment at first diagnosis increased from 61% in 2009 to 71% in 2010, but only from 51% to 53% in patients >75 years. With 26%, WPSS use tripled in 2010 compared to 2009, whereby WPSS was almost always (in 99% of cases) used as an adjunct to and not as a substitute for IPSS.
Cytogenetic testing at first diagnosis stratified by age (2009 n=269; 2010 n=365)
Cytogenetic testing at first diagnosis stratified by age (2009 n=269; 2010 n=365)
In 2010, 22% of all MDS patients did not receive any therapy. Of those treated, 52% received supportive care only, 45% received active treatment (i.e. chemo-, immunomodulatory or epigenetic therapy), 2% SCT, and 1% other treatments. Overall, compared to 2009, the proportion of active treatment remained stable. In the IPSS high risk group, the proportion of active treatment went up from 64% to 96%, declined from 34% to 20% in low risk MDS, but remained stable in patients unclassified by IPSS. In 43% of these patients cytogenetic testing was performed. A significantly lower use of active treatment was still observed in patients >75 years (27% vs. 56%, p<0,0001, fig. 2). As in 2009, the most frequently and increasingly used active drug in 2010 was azacitidine.
Active treatment in the first course of treatment stratified by age (2009 n=200; 2010 n=280)
Active treatment in the first course of treatment stratified by age (2009 n=200; 2010 n=280)
When trying to identify factors driving active treatment, bivariate analysis showed a significant positive correlation with age ≤75 years, hospital as center type, and Karnofsky-index ≤80% (p<0,01). Multivariate analysis revealed age ≤75 years as the most important factor (p<0,001), followed by Karnofsky-index ≤80% (p=0,044).
There seemed to be an increasing awareness and utilization of both cytogenetic testing and IPSS assessment in 2010 vs. 2009. This translated into more frequent use of IPSS for clinical decision making, with a positive correlation between higher IPSS scores and start of active treatment, providing a potential benefit to high risk MDS patients. In patients >75 years, however, IPSS usage remained unchanged despite the increase in cytogenetic testing. It appears that treatment decisions for these patients are more strongly influenced by age and cytogenetics than by IPSS assessment. This leaves room for improvement since under-utilization of prognostic assessment may lead to undertreatment of older MDS patients.
Gattermann:Celgene: Consultancy, Research Funding. Kuendgen:Celgene: Honoraria. Kellermann:Celgene: Consultancy, Research Funding. Zeffel:Celgene: Employment. Paessens:Celgene: Employment. Germing:Celgene: Consultancy, Research Funding.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal