Abstract
Abstract 5097
The uniform response criteria for MM suggest that in clinical practice early biochemical progression (EBP) of MM and clinical relapse (clinREL) be distinguished to identify symptomatic patients requiring therapy. The interval between EBP and clinREL in MM is not well characterized. Biochemical progression in those with intact immunoglobulin MM (IIM) could involve serum free light chain (SFLC) progression or monoclonal component (M spike) progression by serum protein electrophoresis (SPE) or both. ClinREL could precede, be concurrent with or follow tumor marker elevation.
We studied EBP and clinREL in 221 consecutive AHCT recipients for MM between 2005 and 2010. Patients with IIM and measurable M spike and SFLC elevation at diagnosis were analyzed. Patients were uniformly monitored at a single institution with SFLC and SPE every 8–12 weeks. Biochemical progression and clinREL were defined by standard IMWG criteria (Durie el al, Leukemia 2006). ClinREL was defined by new/progressive bone lesion or plasmacytoma, hypercalcemia (>11.5 mg/dl), decrease in hemoglobin ≥ 2 g/dl, rise in creatinine ≥ 2 mg/dl, or indication for new myeloma therapy.
76 patients had clinREL after AHCT, 24 were excluded due to light chain predominant or oligosecretory disease, subsequent AlloHCT or other preemptive treatment. Among 52 evaluable patients, median age was 57 years (42–74), 72% had DSS stage III, 40% ISS stage III, 40% high-risk (HR) MM based on t(4;14), t(14;16), 17q del or karyotypic 13 q abnormality. Median time from AHCT to relapse was 484 days (76–1631).
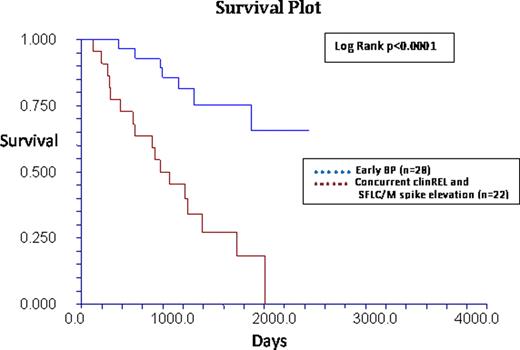
Three temporal patterns of MM recurrence were identified: EBP where SFLC/M spike elevation (or both) preceded clinREL (n=28, 54%); concurrent clinREL and SFLC/M spike elevation (n=22, 42%) or isolated clinREL (4%). The proportion of HR MM was similar among groups. The EBP cohort had superior OS compared to concurrent relapse cohort (log rank p <0.0001).
Additionally in the EBP cohort, SFLC elevation alone (39%), M spike progression alone (22%) or concurrent SFLC and M spike (39%) progression could be the initial relapse marker. After isolated SFLC progression, median time to M spike progression was 112 days and to clinREL was 200 days. After isolated M spike progression median time to clinREL was 254 days. After simultaneous SFLC and M spike progression median time to clinREL was 234 days. In these 3 groups, overall time to clinREL after AHCT was longest for patients with M spike progression alone (17.8, 20.5 and 36.8 months, respectively; p=0.05). This was due to HR MM being more common in the first 2 groups (45% for isolated SFLC and 37% in the simultaneous SFLC/M spike group).
In this cohort of relapsed MM after transplant, 54% had isolated early biochemical progression prior to clinREL and this pattern predicted for superior survival. The category of clinREL may not be detected in advance in about one half of patients and predicts for more aggressive relapse. Present guidelines do not recommend SFLC monitoring for relapse in IIM patients with measurable serum M spike. Based on the above data early SFLC progression was seen in 20% of relapses and identified a higher risk subgroup within those with biochemical progression preceding clinREL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal