Abstract
Abstract 5026
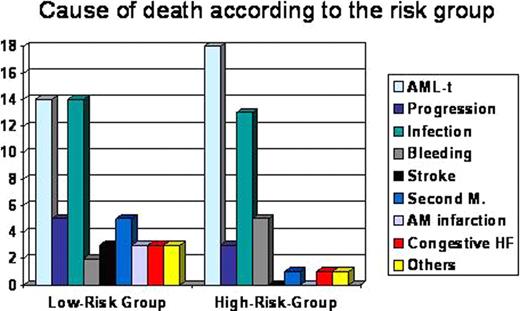
Myelodysplastic syndromes (MDS) are clonal disorders of hematopoietic stem cell with low life expectancy due to several blood cytopenias and high risk of acute myeloid leukemia transformation (AML). Classically, evolution to AML, infection, and hemorrhage are reported as the main causes of death. However, there are few reports analyzing other causes of death in MDS patients, particularly the prevalence of non-MDS-related causes in large series from single-centers. We present here the analysis of causes of death of 200 patients (median age 75yr, range 16–96, 59% male) diagnosed of MDS in our institution between 2000 and 2010. Patients were diagnosed and classified according to the FAB criteria, WHO 2008 classification, IPSS (International Prognostic Scoring System) and SPI (Spanish Prognostic Index). Overall survival (OS) and survival of different MDS subtypes were analyzed. Two prognostic subgroups were defined: low-risk subgroup, composed by patients with low or intermediate-1 IPSS and low SPI; and high-risk subgroup, that included patients with intermediate-2 and high IPSS and intermediate and high SPI. Infection, hemorrhage, disease progression and transformation to AML were considered MDS-related deaths. All other causes of death were classified as non-MDS-related. Median follow-up of the series was 1.8 years (range: 0–11 years). MDS subtypes distribution was as follows: RA, RARS and 5q– 19%; RCMD and RCMD-RS 32%; RAEB-1 and RAEB-2 27%; hypoplastic and unclassified MDS 8%; and CMML 13%. One hundred twenty-nine patients (64.5%) belonged to the low-risk subgroup, whereas 65 patients (32.5%) to the high-risk subgroup. Only 6 patients (3%) could not be classified. Median OS of the whole series was 2 years, being of 3.7 years in the low-risk subgroup and of 0.9 years in the high-risk subgroup (P<0.001). At the time of the analysis, 141 patients (70.5%) had died: 78 (60.4%) of the low-risk subgroup and 59 (91%) of the high-risk subgroup. The cause of death was identified in 97 of 141 (68%) patients and it was related to MDS in 75 patients (77%) and non-MDS-related in 22 patients (23%). In the low-risk subgroup, causes of death were: evolution to AML 14, disease progression 5, infection 14 and bleeding 2. Non-MDS-related causes were: ischemic stroke 3, second malignancy 5, acute myocardial infarction 3, congestive heart failure 3 and others 3. In the high-risk subgroup the causes of death were: evolution to AML 18, disease progression 3, infection 13 and bleeding 5. Non-MDS-related causes were: second malignancy 1, congestive heart failure 1, and accidental 1 (Figure 1). The percentage of patients who died of unrelated-MDS causes was significantly higher in the low-risk subgroup than in the high-risk subgroup (32% vs. 7%, respectively; P=0.003). In conclusion, the most frequent cause of death in both low-risk and high-risk subgroups was related to the MDS (evolution to AML). Non-MDS-related deaths were more common in low-risk subgroup, being the most frequent causes heart failures and second malignancies. Causes of death in MDS should be taking into consideration when analyzing response and survival in clinical trials, particularly when applied to patients belonging to low-risk subgroups.
Disclosures:
No relevant conflicts of interest to declare.
Author notes
*
Asterisk with author names denotes non-ASH members.
© 2011 by The American Society of Hematology
2011

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal