Abstract
Abstract 4854
Patients with Sickle Cell Disease (SCD) are at an increased risk of serious and life-threatening infections. Epstein Barr Virus (EBV) and Human Parvovirus B19 (HPV-B19) are common viral infections that are usually asymptomatic or self-limiting in healthy children. However, SCD patients can have significant morbidity and mortality caused by these infections. In patients with SCD, EBV can cause splenic rupture, thrombocytopenia, agranulocytosis, hemolytic anemia and hemophagocytic lymphocytosis while HPV-B19 can cause severe aplastic crisis, stroke, nephrotic syndrome, myocardial infarction and splenic sequestration. Coinfection with EBV and HPV-B19 has not been reported in SCD patients and there are no reports of EBV or HPV B19 causing septic shock.
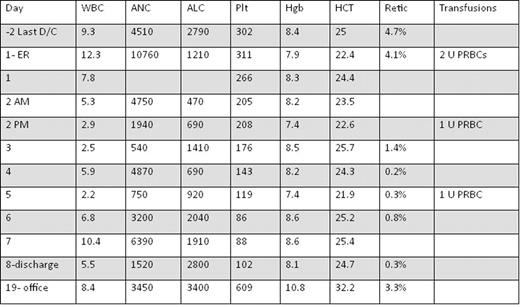
A 15 year old male with SCD presented with a one day history of fever, oliguria, and hypotension caused by simultaneous viremia with EBV and HPV-B19. He had been discharged 2 days previously after an admission for a vaso-occlusive crisis. He did not have pharyngitis, rash hepatosplenomegaly (spleen likely autoinfarcted) or lymphadenopathy. Peripheral smear did not show lymphocytosis, atypical lymphocytes or features of microangiopathic hemolytic anemia. Fluid resuscitation with normal saline and then with red cell transfusion was done and he was transferred to pediatric intensive care unit. He received supportive therapy for septic shock with fluids, antibiotics and red cell transfusions. Blood and urine bacterial cultures were negative and blood quantitative DNA PCR was positive for EBV (3300 copies/ml) and HPV-B19 (2.3×107 copies/ml). His EBV titers were positive for viral capsid antigen (VCA)-IgM and IgG and Epstein Barr nuclear antigen (EBNA)-IgG. He had EBV titers done 2 years previously which were positive for VCA-IgG and EBNA-IgG documenting previous primary EBV infection. The patient gradually improved with supportive therapy and was discharged on Day 8. The patient returned to Pediatric Hematology clinic on Day 19 and had resolution of signs and symptoms. Table 1 shows an overview of his blood counts and transfusion requirements.
Coinfection with EBV and HPV-B19 in healthy adults has rarely been reported. Severe aplastic anemia caused by EBV and HPV-B19 infections was reported in a previously healthy 22-year-old male. He was treated with immunosuppressive therapy followed by allogeneic bone marrow transplant (Kaptan K et al, Am J Hematol 2001). Acute HPV-B19 infection and concomitant EBV reactivation causing moderate hemophagocytic syndrome was reported in a previously healthy 37-year-old-male (Larroche C et al, Eur J Clin Microbiol Infect Dis 2002). HPV-B19 infection with EBV reactivation has not been reported in children.
Sepsis from viremia is not common with either EBV or HPV-B19, however together this co-infection can be life-threatening as seen in our patient. HPV-B19 infection has been reported to produce false positive EBV VCA-IgM serology assay. Our patient had a true coinfection because he had viremia documented by EBV DNA PCR.
This is the first report of viremia and septic shock associated with an acute HPV-B19 infection and EBV reactivation in a patient with SCD.
WBC- White Blood Cell Count, ANC- Absolute Neutrophil Count, ALC- Absolute Lymphocyte Count, Plt- Platelet Count, Hgb- Hemoglobin, HCT- Hematocrit, Retic: Corrected Reticulocyte Count, U- Units, PRBC- Packed red blood cells, ER- Emergency room
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal