Abstract
Abstract 4838
Regularly transfused patients including those with MDS and AA inevitably accumulate iron in various tissues, hence the importance of iron chelation to prevent end organ dysfunction. Studies of iron chelation in MDS and AA have mostly used serum ferritin as an efficacy indicator; LIC data, a more direct measure of clinical benefit are limited in these patients. Here, we report results from a 1-year Phase II, multicenter study evaluating the effect of deferasirox (DFX) on LIC in iron-overloaded patients with MDS, AA, and other rare anemias.
Patients aged ≥2 yrs with transfusional iron overload due to low/intermediate (Int-1) risk MDS, AA and other congenital or acquired anemias were enrolled. Patients with thalassemia and SCD were excluded. Patients required a lifetime transfusion history of ≥20 units of packed red blood cells (RBC) or serum ferritin >1000 ng/mL. DFX was administered at a starting dose of 20 mg/kg/day; some patients started on 10 or 30 mg/kg/day based on transfusion requirements and therapeutic goals. Dose adjustments were based on serum ferritin trends and safety parameters. Primary endpoint was absolute change in LIC assessed by R2 MRI (Ferriscan®) from baseline (BL) to 1 year. Secondary objectives included analyses of change in serum ferritin, iron balance and safety.
102 patients (MDS n=42 [41.2%], AA n=29 [28.4%] and other rare anemias n=31 [30.4%]) were enrolled. Median age was 56.5 yrs (range 2–85 yrs). 68 (67%) patients completed 1 year of treatment. Average actual dose (mean ± SD) was 18.5 ± 5.6 mg/kg/day; 64 patients (62.7%) received an average dose of 15–<25 mg/kg/day.
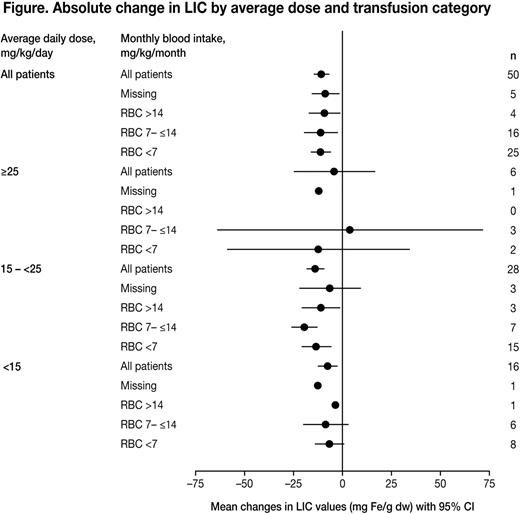
Mean ± SD BL LIC was 24.5 ± 15.6 mg Fe/g dw (n=102); with 23.5% (n=24) and 56.9% (n=58) of patients having LIC >7–<15 and ≥15 mg Fe/g dw, respectively. Median BL serum ferritin was 2999 ng/mL (range 110 to 27,550). For patients with evaluable LIC at BL and 1 year (per protocol set, n=50), mean LIC decreased significantly from 25.6 at BL to 14.7 at 1 year (–10.9 mg Fe/g dw, [95% confidence interval [CI]–14.3, –7.5], relative change 42.9%). Median serum ferritin decreased by –684 ng/mL (range –11,150 to 29,400) from a BL of 2999 (range 110 to 27,550) to 2057 ng/mL (range 193 to 30,800) at 1 year. Reductions in LIC and serum ferritin were observed across dose categories and blood transfusion requirements and were more pronounced in patients receiving RBC <7 and 7–≤14 mL/kg/month (Figure). There was a correlation between relative change in LIC and relative change in serum ferritin (R=0.606, per protocol set) and relative change in LIC and relative change in ALT (R=0.457, per protocol set). Overall, mean iron balance (Fe excretion/Fe intake) was +2.46 (n=45).
Most frequent (≥5%) adverse events (AE) suspected by the investigator to be drug-related were increased blood creatinine (n=19, 18.6%), skin rash (n=9, 8.8%), renal impairment (n=8, 7.8%), diarrhea (n=7, 6.9%), nausea (n=7, 6.9%), abdominal pain (n=6, 5.9%) and constipation (n=6, 5.9%). 14 severe AEs suspected to be drug-related were reported in 10 patients, the most frequent (≥2) being rash (n=2) and hypersensitivity (n=2). Five patients died (general physical health deterioration [n=2], cerebellar hemorrhage, disseminated intravascular coagulation and traumatic hemorrhage [n=1 for each]); none were considered drug-related. Cataract was reported in 4 patients (3.9%); 1 suspected as drug-related. Auditory AEs were reported in 7 patients; aggravated deafness (n=1) and tinnitus (n=1) suspected to be drug-related. Of 19 patients treated with concomitant cyclosporine (CyA), 11 (57.9%) had increases in serum creatinine (>33% above BL and >ULN at 2 consecutive visits) compared with 18 of the remaining 83 patients (21.7%) who did not receive CyA.
A large proportion of patients in this study with transfusion-dependent Low/Int-1 risk MDS, AA and other rare anemias had severe liver iron overload (LIC ≥15 mg Fe/g dw). 1 year of DFX treatment significantly reduced iron burden, as assessed by both LIC and serum ferritin; with iron excretion 2–3 times higher than iron intake. Furthermore, change in LIC correlated with change in serum ferritin and ALT, a clinically relevant indicator of liver function. Overall the DFX safety profile was consistent with that from previous studies. Renal function in patients receiving DFX and concomitant CyA should be closely monitored as previously noted in the EPIC trial.
Kohgo:Kyorin Pharma: Research Funding; Sapporo Brewery: Research Funding; Asahikasei Kurare Medical: Research Funding; Chugai Roche: Research Funding; Novartis: Research Funding, Speakers Bureau. Sanz:Novartis: Speakers Bureau. Helou:Novartis: Employment. Habr:Novartis: Employment. Malet:Novartis: Employment. Glaser:Novartis: Employment. Wiktor-Jedrzejczak:Novartis: Honoraria, Research Funding; Janssen-Cilag: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal