Abstract
Abstract 4676
Bernard Soulier Syndrome (BSS) is a rare qualitative and quantitative autosomal recessive platelet disorder molecularly characterized by defective GPIb-IX-V membrane glycoprotein that is related to platelet adhesion and interaction with both Von Willebrand factor and endothelium. It is usually expressed by an enlarged bleeding time and decreased yet giant sized platelets, and can cause severe hemorrhagic complications during pregnancy.
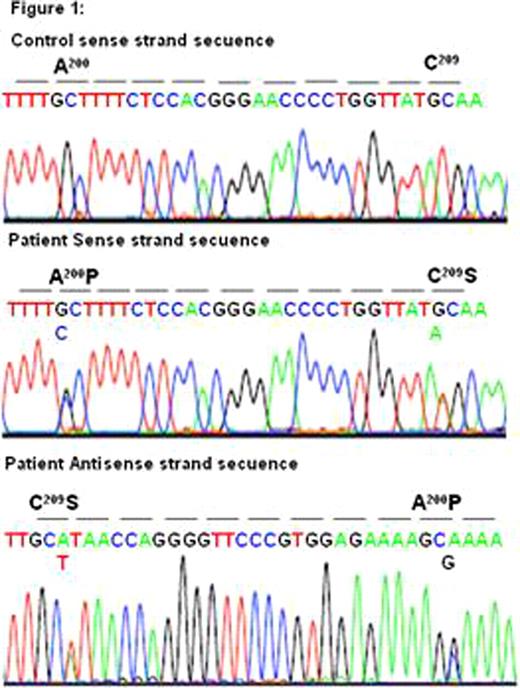
We present two successful pregnancies and labour management on a 33-year-old woman diagnosed in her childhood with BSS. Ristocetin induced platelet agglutination test and membrane glycoprotein study were performed to get the diagnosis. Furthermore, in the last year we have completed the diagnosis with platelet receptor expression flow citometry analysis, finding out depleted antiGPIbα and antiGPIX antibodies. Changes which prevent GPIbα for correct expression and processing were observed. Also integrin αIIbβ3 levels were risen due to the big sized platelets. A PCR product was obtained from genomic DNA using the GPIbα oligonucleotide pair; sense and antisense, and direct DNA sequencing of the amplification was performed in a model ABIprism 377 DNA sequencer (Perkin-Elmer Cetus). The direct sequencing of the sense strand of the 5x fragment shows in the patient the simultaneous presence of G and C nucleotids in 688 position, and the T and A nucleotids in 715 position. These punctual mutations give Ala200Pro substitutions and Cys209Ser in heterozygosis in mature peptide, respectively, Figure 1. The Ala200Pro mutation has not been reported in others cases of Bernard-Soullier, previously. The Cys209Ser has been described in other two Spanish patients: one in homozygosis and the other in heterozygosis associated to the mutation.
Our patient presented hemorrhagic symptoms from 18 month old with an average of 40×103/μ l platelet count and increased platelet volume who required multiple platelet transfusions during her childhood. In the menarche main hemorrhagic manifestations consisted on methrorragia and epistaxis which were controlled with tranexamic acid. At the age of 26 a spontaneous ovarian cyst rupture required urgent hospital admission and two platelet pool transfusion. On December 2007 she consulted for epistaxis, and on September 2008 cesarean delivery was planned at 38th week of pregnancy; platelet count was 40×103/μ l, antiplatelet antibodies were negative for membrane glycoproteins and antiHLA-1 was positive against 98% donors tested. As a result, an HLA-compatible donor was searched, and two platelet apheresis were transfused one hour before surgery and every 12 hours after the procedure. The next 4 days one apheresis every 48 hours were transfused with no hemorrhagic symptoms. On January 2010, she presented with her second pregnancy; the patient had severe anemia, with high transfusion requirements; neither hemorrhage or hemolysis was detected, and even the possibility of a Munchausen syndrome was questioned. Unplanned caesarean was performed at 32th week because of the clinical instability of the patient, and this time we could not find on time an HLA-compatible donor, so two random platelet pools were transfused one hour before surgery and one platelet apheresis every day during 4 days after caesarean deliver, without any hemorrhagic complication. The newborn was asymptomatic with normal platelet count. The patientxs haemoglobin level returned to normal after five days of delivery.
We present the successful labour management of two consecutive pregnancies on a young woman diagnosed with BSS. The low prevalence of this syndrome (less than one case per million population) explains the absence of well-established protocols for the management of pregnancy in this disease. Up to date there are only twelve reported cases of pregnancy and delivery in BSS patients, most of them presenting with severe hemorrhagic complications. Correct platelet transfusion is the mainstay of treatment, and screening for anti-platelet antibodies study is mandatory due to its high prevalence in these patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal