Abstract
Abstract 4604
Chronic lymphocytic leukemia (CLL) has the highest incidence and prevalence of any leukemia in the United States. It has a characteristic immunophenotype, but variant forms (typically termed “atypical CLL”) are commonly encountered. It is not known if this immunophenotypic heterogeneity in CLL is clinically relevant. We hypothesized that the immunophenotype of CLL cells correlates with both biologic parameters and clinical outcomes.
We performed a retrospective review of clinical, biologic, and flow cytometric data of patients undergoing an evaluation of an absolute lymphocytosis at the Duke University and Durham VA Medical Centers. Patients meeting immunophenotypic criteria for CLL based on cell surface expression of CD5, CD19, CD20, CD23, and surface immunoglobulin light chain (sIg) were included in this analysis. Atypical CLL was defined if any of the following were observed: (1) expression of CD5, CD20, CD23, or sIg that differed from a typical CLL immunophenotype (e.g. bright CD20 or low CD23; hereafter non-standard immunophenotype), (2) expression of T cell markers CD7 or CD8, or (3) expression of CD123. Through electronic chart review, clinical and biologic parameters were abstracted. These included age; gender; ethnicity; WBC, hemoglobin, platelet count, and Rai stage at diagnosis; time to first treatment; overall survival; CD38, ZAP70, IGHV mutation status, and interphase cytogenetics (FISH). A chi square test or Fisher’s exact test for small sample sizes was used to test association of categorical data. The central tendencies of continuous measurement were compared using the Wilcoxon rank sum test. Overall survival and time to treatment were calculated using the Kaplan-Meier product limit method. Survival curves were compared using the log-rank test. This study was approved by IRBs at Duke University and Durham VA Medical Centers.
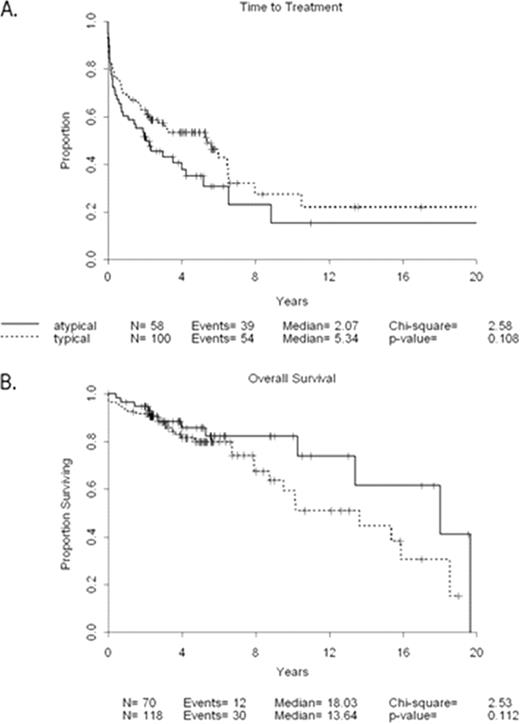
We reviewed 189 patients, including 119 (63%) with typical CLL immunophenotype and 70 (37%) with atypical. Among patients with atypical CLL, 93% (65 of 70) had a non-standard immunophenotype, 33% (23 of 70) had expression of T cell markers, and 33% (14 of 43) had expression of CD123. We observed expression of T cell markers in 12% (23 of 189) and CD123 in 12% (14 of 114) of the entire cohort, respectively. At the time of diagnosis, there was no association between typical or atypical CLL immunophenotype and age, gender, race/ethnicity, WBC, hemoglobin, platelet count, or Rai stage (p>0.05 for all comparisons). With regard to biologic parameters, there was no association of CLL immunophenotype with the proportion of patients with CD38 ≥30%; however, the central tendency of CD38 was higher in the atypical group when analyzed as a continuous variable (median value 38% vs. 10%, p=0.04). There was no difference in the proportion of ZAP70 positive cases between typical and atypical groups. Analysis of interphase cytogenetics (FISH) data showed that a higher percentage of typical than atypical immunophenotypes had del 13q as a sole abnormality and a lower percentage had trisomy 12 (p=0.02). Despite the increased frequency of del 13q as a sole abnormality, lower frequency of trisomy 12, and lower expression of CD38, there was no difference between groups in time to first treatment (median 5.3 years for typical vs. 2.1 years for atypical; p= 0.11) or in overall survival (median 13.6 yrs64 years for typical vs. 18.0 years for atypical; p=0.11) (Figure 1). However, when patients with non-standard CLL immunophenotype were compared to those with a standard immunophenotype, a significantly shorter time to first treatment was observed (median 6.0 years for standard immunophenotype vs. 2.2 years for non-standard, p=0.03).
Different immunophenotypic subtypes are commonly encountered in the care of patients with CLL. These groups have different biological characteristics, including differences in expression of CD38 and cytogenetic abnormalities. Exploratory analysis also showed differences in clinical outcomes based on immunophenotypic parameters. Validation studies are currently underway.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal