Abstract
Abstract 4538
Following hematopoietic stem cell transplantation (HSCT), morbidity and mortality are often related to opportunistic infection early post HSCT and it is accepted that immune reconstitution has a protective effect. Absolute lymphocyte counts (ALC) act as a surrogate for immune reconstitution. Prior studies suggest that an ALC greater than 0.5×10^9/L on day 15 post autologous HSCTs and greater than 0.3×10^9/L on day 30 post allogeneic HSCTs can prognosticate overall survival (OS) and progression-free survival (PFS). However, most of these studies have been single disease small studies. We designed this study to evaluate whether patients with a wide variety of diseases undergoing either autologous or allogeneic HSCT at Thomas Jefferson University Hospital would fit this model or if other cut-points were more appropriate.
Data was abstracted from the charts of 585 HSCTs (265 autologous, 320 allogeneic (228 HLA identical and 92 haplo-identical) preformed consecutively between January 1999 and April 2009. Prior treatments, disease status at time of HSCT, conditioning regimens, and progression-free and overall survival were collected. Survival methods (Kaplan-Meier and logrank test, and Cox proportional hazards regression) were used to analyze PFS and OS as a function of ALC and other clinical variables. Separate models were fit for ALC counts on day 15, day 30, and day 90 post-transplantation, as predictors of PFS (or OS). ALC was categorized as less than or equal to 0.5 or greater than 0.5 ×10^9/L. The possibility of differential association between ALC counts and PFS (or OS) among autografts versus allografts was tested by including interaction terms between ALC counts at each time point and graft type.
For these analyses, we excluded third and fourth HSCTs (n = 4), as well as the first of tandem autologous/allogeneic HSCTs (n = 26) and the first of two HSCTs that were performed during the same admission (n = 8). We also excluded HSCTs for which ALC counts on admission or on day 15 post-HSCT were not available (n = 14). Therefore, these analyses were based on data for a total of 532 HSCTs, including 443 first HSCTs and 89 second HSCTs.
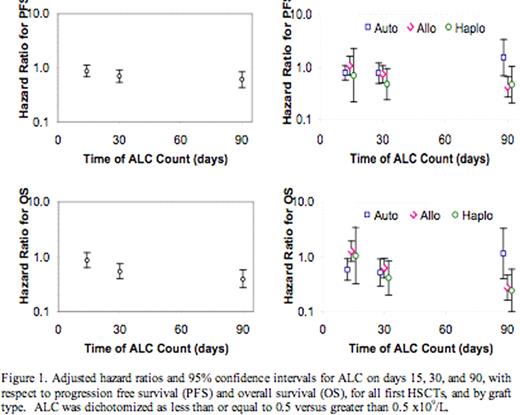
Adjusted hazard ratios and 95 confidence intervals for ALC on days 15, 30, and 90, with respect to progression free survival (PFS) and overall survival (OS), for all first HSCTs, and by graft type. ALC was dichotomized as less than or equal to 0.5 versus greater than 0.5 ×109/L.
Adjusted hazard ratios and 95 confidence intervals for ALC on days 15, 30, and 90, with respect to progression free survival (PFS) and overall survival (OS), for all first HSCTs, and by graft type. ALC was dichotomized as less than or equal to 0.5 versus greater than 0.5 ×109/L.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal