Abstract
Abstract 4531
Many recent advances have occurred in the field of MDS including hypomethylating agents, lenalidomide, and WHO classification. Likewise the field of hematopoietic stem cell transplantation has also undergone major new developments including improved supportive care, high resolution HLA typing, allowing better selection of unrelated donors, and development of reduced toxicity conditioning regimens like Busulfan and Fludarabine. The role of HCT needs to be reexamined in light of these developments. We report long-term data on patients transplanted over a seven-year period and analyze prognostic factors.
89 consecutive patients with MDS as defined by WHO criteria treated at our institution between Jan 2002 and April 2008 are included in this report. There were 60 males and 29 female with a median age of 54 (23–67). There were 6(7%) patients with RA or RARS, 8 (9%) RCMD, 23(26%) RAEB 1, 17(19%) RAEB 2, and 35 (39%) therapy related MDS (t MDS). Cytogenetic groups were Good risk 33(37%), intermediate 13(14%), poor 43(48%) per IPSS criteria. Conditioning regimens were myeloablative fludarabine and Busulfan (Flu/Bu) in 53 (60%), reduced intensity Flu/Bu 3 (4%), reduced intensity fludarabine/melphalan 32 (36%), Bu/Cy 1 (1%). Donors were matched siblings for 51 patients and matched unrelated for 38. According to HCT-CI index, the comorbidity scores were 0 in 16 (18%) patients, 1 or 2 in 19(21%) and greater then 2 in 54(61%). Median time from diagnosis to transplant was 8 months (range 1– 51 months). Median follow up of survivors was 4.1 years.
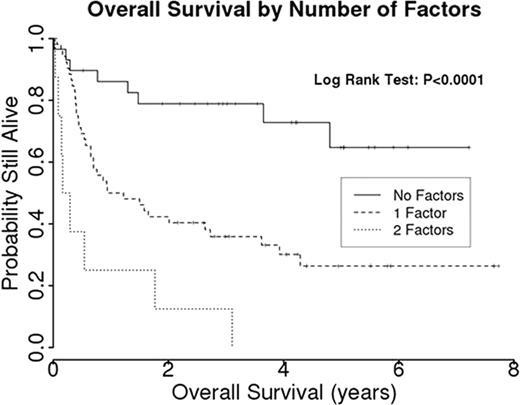
Overall survival (OS) and disease free survival at 3 years were 48%(95% CI; 37%-58%) and 43% (32%-53%) respectively. Cumulative incidence of non relapse mortality at 3 years was 26% (17%-36%). Cumulative incidence of relapse at 3 years was 31% (21%-41%). Univariate analysis showed that cytogenetic group (P<0.001) and bone marrow blast count were predictive of overall survival, but age, sex, conditioning regimen, stem cell source, donor type, prior treatment, prior remission status, and WHO category did not impact survival. Multivariate analysis showed that bone marrow blast count > 10% and intermediate or poor risk cytogenetics were significantly predictive of inferior survival. A prognostic model using presence or absence of these factors was significantly predictive of OS (fig). 3 year OS with 0, 1, or 2 of these factors was 79%, 36%, and 12%, respectively.
Allogeneic transplantation induces long term remission in patients with MDS. High (>10%) bone marrow blast count and intermediate or poor risk cytogenetics are adverse prognostic factors.
Popat:Otsuka: Research Funding. Qazilbash:Otsuka: Research Funding. Andersson:Otsuka American Pharmaceuticals, Inc.: Consultant for Clinical Protocol Development. Champlin:Otsuka: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal