Abstract
Abstract 4530
The treatment of acquired SAA is based on allogeneic stem cell transplantation (SCT) and immunosuppressive therapy. Up to 68% of patients in our country are treated without transplantation, and in our hospital a preliminary report (1999–2006) shows that 56% of these patients have achieved partial or complete response. Peruvian patients with aplastic anemia usually present poor prognosis factors, such as more than 6 months of diagnosed disease before transplantation (53%) and more than 15 RBC transfusions before the procedure (69%). The aim of this study was to assess the outcome of children and adults with SAA, treated with related allo-transplant and the evolution of patients with poor prognosis factors in Hospital Rebagliati (Lima, Peru - 1995 to 2010).
Retrospective and Descriptive analysis where was included variables related to the patients, disease and method of transplantation in 88 patients of the 95 who went to transplant.
The median age at diagnosis was 26 years (3–55 years), male/female ratio: 1.75, the interval between diagnosis – SCT was 12.7 months (1–151 months), in 47.7% of patients this interval was ≤ 6 months. GVHD prophylaxis consisted of CsA + MTX. The conditioning regimen was ALG equine or rabbit (based on availability), + cyclophosphamide in 95% of patients and cyclophosphamide + busulphan in 1%; 59 patients received equine anti-lymphocyte globulin and 27 patients received rabbit anti-lymphocyte globulin. The stem cell source was bone marrow in 35.2% (31), peripheral blood in 58% (51), bone marrow and peripheral blood in 5.7% (5) and umbilical cord blood 1.1% (1). Two of the 88 patients required a second transplant and continue alive.
The stem cell source did not show a significant difference in the time to neutrophil engraftment (p=0.15), which took place around day 13 (10–28 days). The dose of MNC used was 3×108/kg when BM was the graft source and CD34 > 2×106 if the source was peripheral blood. The engraftment was done all patients (n:88).
The mortality rate was 19.4% after BMT, despite the number of RBC transfusions and mostly due to lost of engraftment, and 9.8% after using peripheral blood as the graft source.
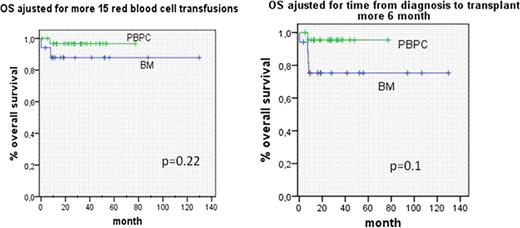
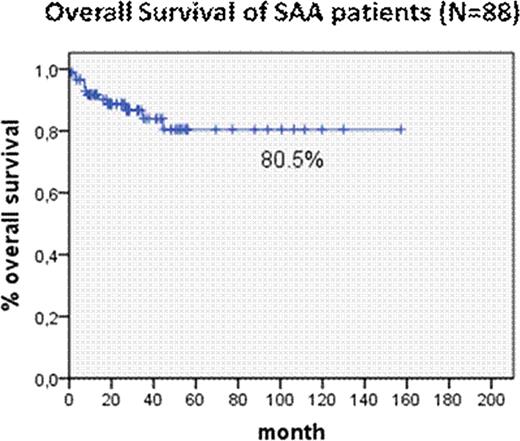
The overall survival was 80.5%, this patients were followed for a period up to 157 months. There was not a significant difference in survival with the use of bone marrow or peripheral blood as the stem cell source (p=0.2); nonetheless, we observed a trend toward better survival rates when performing PBSCT, according to the time interval between diagnosis to SCT and the number of transfusions.
The kind of anti-lymphocyte globulin –horse or rabbit origin- used, did not show a major impact in survival (p=0.13). A major predictor of a significantly improved HSCT outcome in Peru, was the development of acute GVHD (p=0.03).
OS is 80%, superior compared with immunosuppressive therapy alone (56%). The presence of acute GVHD is a major predictor of survival in those receiving SCT. The use of peripheral blood as the stem cell source seems to improve survival in Peruvian patients with poor prognosis factors, in comparison with the use of bone marrow source.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal