Abstract
Abstract 4254
Invasive fungal infections (IFI) are a significant cause of morbidity and mortality in patients with acute myelogenous leukemia (AML) undergoing chemotherapy treatment. However, the epidemiology, risk factors, and outcomes of IFI in these patients have been poorly described.
A single-center retrospective analysis was performed to study the epidemiology, risk factors, clinical outcomes, and mortality predictors of IFIs in AML patients undergoing intensive, multi-agent induction timed sequential therapy (TST) between January 2005 and June 2010. Newly diagnosed AML patients, with exception of acute promyelocytic leukemia, were studied. IFIs were defined using the European Organization for Research and Treatment of Cancer/Mycoses Study Group (EORTC/MSG) criteria.
254 consecutive patients (57% male; median age 54, range 20–78) were analyzed. 123 (48%) of patients had an IFI; of which, 15 patients (12%) had a proven candidal infection, and 108 patients (88%) had a mould infection (5 proven/probable (5%) and 103 (95%) possible mould infections). 237 (93%) patients received antifungal therapy during their treatment course (median day 8, range day -15 to 30). Of those, 63 (27%) received monotherapy (46% liposomal amphotericin, 44% voriconazole) and the rest received multiple antifungal agents.
Significant risk factors and trends for developing +IFI shown from univariate analyses are listed in Table 1. Prolonged neutropenia, duration of mucositis, and concurrent bacterial infections did not significantly affect the development of +IFI. Using multivariate analyses, mortality was impacted by patients’ baseline organ function (p=0.002 [1.3,3.1]), specifically, by bilirubin < 2 mg/dL (p=0.003 [1.38,4.57]) and creatinine < 1.5 mg/dL (p=0.01 [1.23,5.4]).
Significant risk factors and trends for development of + IFI
| . | No IFI . | + IFI . | P-value . |
|---|---|---|---|
| Male Gender (%) | 50 | 64 | 0.023 |
| Leukemia from a secondary cancer (%) | 15 | 4 | 0.003 |
| Duration of parenteral nutrition (days)* | 9.5 | 17 | 0.057 |
| Candida Colonization (%) | 85 | 93 | 0.043 |
| Grade 3+ mucositis (%) | 42 | 59 | 0.05 |
| . | No IFI . | + IFI . | P-value . |
|---|---|---|---|
| Male Gender (%) | 50 | 64 | 0.023 |
| Leukemia from a secondary cancer (%) | 15 | 4 | 0.003 |
| Duration of parenteral nutrition (days)* | 9.5 | 17 | 0.057 |
| Candida Colonization (%) | 85 | 93 | 0.043 |
| Grade 3+ mucositis (%) | 42 | 59 | 0.05 |
values are median days
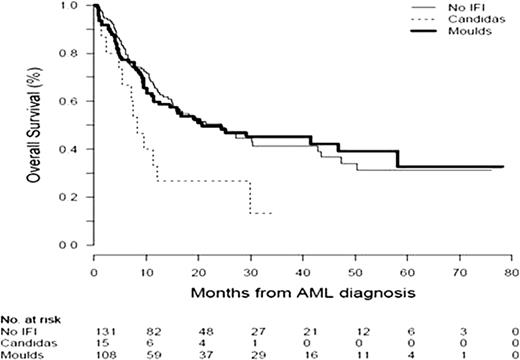
Patients with +IFI did not significantly impact overall survival. However, patients with candidal IFIs had a significantly lower overall survival compared to patients with mould IFIs and no IFI (HR 2.01 [1.06, 3.8]) (Figure 1). Candida colonization prior to or during the first week of chemotherapy, and development of mucositis were associated with the development of candidal IFIs (p=0.07).
IFIs, particularly mould infections, remain a significant problem in patients with AML. Although overall survival did not appear to be significantly affected by mould infections, patients with candidal infections were more likely to die. Identification of risk factors for each type of IFIs may help to develop effective targeted preventive antifungal strategies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal