Abstract
Abstract 3978
Bortezomib alone and in combination with other agents has shown great promise in the treatment of AL amyloidosis in various preliminary open studies. Here we present our experience at the UK National Amyloidosis Centre with CVD in both the upfront and relapsed setting.
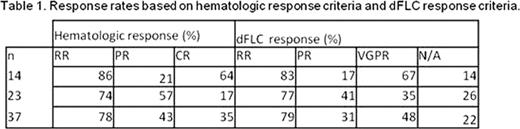
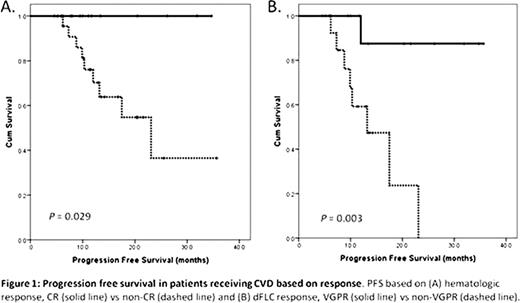
The primary cohort comprises 37 patients referred to the National Amyloidosis Centre in London from 2006–2010. 27 patients had cardiac involvement by 2005 consensus criteria. 29 had renal involvement, 10 had liver involvement and 26 had other organs involved. Complete information for staging by the Mayo clinic criteria was available in 34 patients, and 47% were stage III based on values obtained prior to the initiation of CVD (23% of upfront patients and 62% of relapsed patients). The recommended CVD regimen was as follows: bortezomib 1.0 mg/m2 IV days 1, 4, 8, 11 (increase to 1.3 mg/m2 if well tolerated) cyclophosphamide 350 mg/m2 po days 1, 8, 15 dexamethasone 20 mg po days 1, 4, 8, 11 (increase to 40 mg if well tolerated) with an aim to deliver 6 cycles of treatment. Dose modifications were at the discretion of the treating haematologist. We aimed to assess response at 6 months (m). Haematologic and organ responses were defined as per the 2005 consensus criteria. The dFLC response (difference between the involved and uninvolved free light chain) was defined as the percent difference in the dFLC at the start of therapy and at response assessment and was considered assessable if the baseline dFLC was >50mg/L. A dFLC of 50–90% defined a partial response, and a dFLC of >90% defined a VGPR. Progression free survival (PFS) was calculated by the Kaplan-Meier method and calculated from the start of CVD until relapse, death or last follow-up. Statistical analysis was performed using SPSS version 19. Approval for analysis and publication was obtained from the institutional review board at the University College London, and written consent was obtained from all patients.
Median follow-up was 13.3m. Median time to assessment was 5.9m. Median number of cycles given was 4.9. All 37 patients were assessable by haematologic response criteria, 29 of whom were assessable for dFLC response. Overall hematologic response rate (RR) was 78.4% (CR = 35.1%). A VGPR was attained 48.3% of patients with an overall dFLC RR of 79.3%. 14 patients were treated with CVD upfront with a RR of 85.7% (CR = 64.3%, VGPR = 66.7%). 23 patients were treated in the relapse setting and the RR was 73.9% (CR = 17.4%, VGPR = 35.3%). Clonal response is detailed in table 1. 26 patients were assessable for a BNP response based on a pre-treatment NT-proBNP > 660 ng/L. BNP responses were seen in 8 patients (31%), stable disease in 14 (54%) and progression in 4 (15%). Of the entire cohort only one death was reported and there were no treatment related mortalities. The time to maximal response was 3.8m (3.0m and 3.8m in patients treated upfront and at relapse respectively). Median PFS has not been reached. The estimated 2-year PFS was 55.6% for the entire cohort, 69.6% for patients treated upfront and 43.8% for those treated at relapse. Attaining a CR correlated with a significant improvement in progression free survival compared with those who had not (median PFS not reached vs. 23.1m respectively, P = 0.029; figure 1A). Attaining a VGPR also correlated with an improved PFS compared with those who had not (median PFS not reached vs. 13.2m respectively, P = 0.003; figure 1B).
This retrospective series lends further support to the use of bortezomib containing regimens in the treatment of AL amyloidosis. CVD is a safe and effective treatment option supporting similar findings in other small retrospective series, particularly when used in the upfront setting. This is, to our knowledge, the first series reporting PFS with this regimen. In addition, it confirms the importance of achieving a CR for improved survival outcomes and further validates the dFLC response as an important treatment endpoint. CVD is an attractive treatment combination for patients with AL amyloidosis many of whom are transplant ineligible due to advanced disease. Larger phase III studies are warranted and are underway.
Wechalekar:Jansen Cilag: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal