Abstract
Monoclonal B-Cell Lymphocytosis is an asymptomatic hematologic condition characterized by the presence of small populations of clonal B-cells in the blood or bone marrow occurring in 3–5% of the general population over age 40. Although MBL is considered the precursor state to CLL and other sub-types of indolent non-Hodgkin Lymphoma, most individuals with MBL will not develop a B-cell malignancy. It is unknown, however, whether individuals with MBL may be at risk for other adverse outcomes associated with CLL, such as increased risk of infection. To explore this aspect, we evaluated the risk of hospitalization for infection among patients with clinically recognized MBL and compared this to a cohort of general medicine patients and a cohort of CLL patients.
The Mayo Clinic Rochester (MCR), a tertiary referral center in rural southeastern Minnesota, is also the primary hematology center for southeastern Minnesota, northern Iowa, and western Wisconsin. There are no metropolitan areas or hematology specialty centers within a 50 mile radius. To explore the natural history of infection in a local, community dwelling cohort of individuals with clinically identified, CLL-phenotype MBL, we used the Mayo Clinic CLL database to identify all patients with newly diagnosed MBL seen in the MCR Hematology Division between January 1999 and December 2009. Analysis was limited to MBL cases who resided within 50 miles of MCR. The comparison cohort consisted of 689 adult patients also resided within 50 miles of MCR who were seen for a general medical examination between September 2002 and December 2009 and who were enrolled as controls in a case-control study of non-Hodgkin lymphoma. Rates of infection among individuals with MBL were also compared to a cohort of 174 patients with newly diagnosed CLL diagnosed in the same time interval and who resided within 50 miles of MCR. All hospitalizations in these 3 groups were audited to document hospitalization with infection including cross-referenced with the electronic Mayo Clinic infection database, which contains all culture results obtained from hospitalized patients at MCR. Serologies and viral assays (e.g. CMV viral load) were also reviewed. Patients whose cultures were negative but who were given a clinical diagnosis of infection (e.g. pneumonia) and who were treated with a full course of antibiotics were considered to have a culture negative infection. Among the cases, only hospitalizations after CLL or MBL diagnosis were considered.
In May 2010, there were 524 individuals in the Mayo Clinic MBL/CLL Database with the diagnosis of CLL-phenotype MBL made between January 1999 – December 2009. Of these, 154 (29%) patients resided within a 50 mile radius of Mayo Clinic and were considered a local, community-based cohort of MBL patients. Median age at MBL diagnosis for these 154 patients was 70 years (range 45–94).
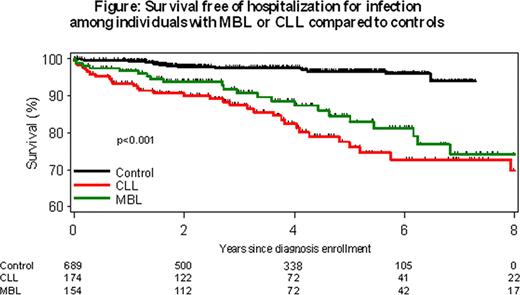
After median follow-up of 4.2 years (range 0.3–10.6 years), 25 (16%) individuals with MBL were hospitalized with infection as compared to 20/689 (3%) individuals in the control population (odds ratio MBL relative to control=6.5; p<0.001) and 32/174 (18%) in the cohort of patients with newly diagnosed CLL (OR MBL relative to CLL=0.9; p=0.61) (Figure 1). The 25 MBL patients hospitalized for infection were hospitalized a total of 39 times (median 1 hospitalization for infection per individual). A specific infectious organism was identified by cultures or serologies in 8/39 (21%) hospitalizations among individuals with MBL, 10/27 (37%) hospitalizations for infection among controls, and 60 (63%) of the 89 hospitalizations for infection in CLL cases.
Finally we performed a pooled multivariable analysis of all patients (n=1017) adjusting for age, sex, presence of MBL, diagnosis of CLL, and whether patients with CLL or MBL received treatment for CLL during follow-up. All factors were independently associated with risk of hospitalization for infection [Age (per year, OR=1.02, p=0.02), sex (male, OR=2.6, p=0.001), presence of MBL (OR=3.3, p<0.001), diagnosis of CLL (OR=3.0, p=0.002), and treatment for CLL (OR=3.3, p<0.001)].
In this cohort study, patients with newly diagnosed clinical-MBL had a 6.5 fold risk of hospitalization for infection relative to the control cohort. MBL was an independent risk factor for hospitalization for infection after controlling for age, sex, and treatment.
Zent:GlaxoSmithKline: Research Funding; Genentech: Research Funding; Genzyme: Research Funding. Kay:Biothera: Research Funding; Clegene: Research Funding; Cephalon: Research Funding; Genentech: Research Funding; Glaxo Smith Kline: Research Funding; Hospira: Research Funding; Novartis: Research Funding; Supergen: Research Funding; Calistoga: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Emergent Biosolutions (Formerly Trubion): Membership on an entity's Board of Directors or advisory committees.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal