Abstract
Abstract 3794
CMML is a heterogeneous disease with overall survival (OS) ranging from 12 mo to several years, where few series of allo-SCT have been published. This retrospective study aimed at determining prognostic factors for OS after allo-SCT in a group of consecutive 73 CMML patients reported to the SFGM-TC registry between 1992 and 2009.
For this analysis, in addition to classical demographic and transplant characteristics, patient data at diagnosis and at transplant, including WHO classification in CMML 1 and 2, IPSS in patients with WBC <13G/L, and prognostic factors published by the Groupe Francophone des Myélodysplasies (GFM) in CMML with WBC >13G/l (unfavorable factors included: palpable splenomegaly (SPM), Hb<10g/dl, Platelets<100G/l, marrow blasts>5%, abnormal karyotype, extramedullary disease) (Wattel et al, Blood 1996, 88:2480, Braun T., Blood 2011, online), interval between diagnosis and allo-SCT, and prior treatment were analyzed.
Patient characteristics at diagnosis were as follows: M/F 49/26, median age 53 yrs (range, 27–66). 30% pts had palpable SPM, 70% WBC>13×10^9/L. 48/12/9 pts had good/int/poor risk karyotype according to IPSS, including normal (n=47), monosomy 7 (n= 7) and abn 8 (n= 5). 61%pts had CMML1, and 39% CMML-2. Of the 22 patients with WBC<13G/l, six had int-2 and 1 had high risk IPSS, while of the 45 patients with WBC>13G/l, 37 had at least 2 of the GFM poor prognostic factors (see above). Before allo-SCT, 26 pts had received intensive anthracycline-cytarabine chemotherapy (CT), 21 low dose CT (18 HY, 3 VP16) and, 6 hypomethylating agents. Forty pts (56%) developed infection (bacterial or fungal) between diagnosis and allo-SCT.
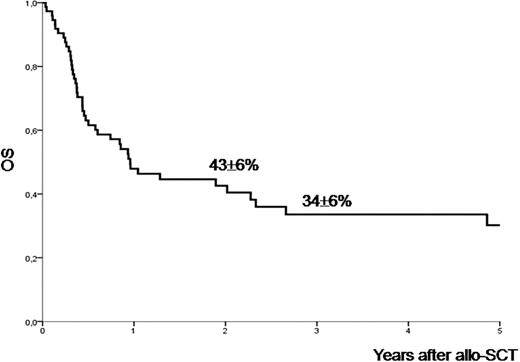
Median interval from diagnosis to allo-SCT was 10.6 mo (range 2.8–80). At time of allo-SCT, 26 pts (49%) had responded to therapy (19 CR and 7 PR), while 42 pts were treatment failure or in relapse, or had not been treated, including 5 AML progressions, (80% CMML1 and 13% CMML 2, while, in 52 pts with WBC <13 G/L, 8 and 6 had IPSS int-2 and high respectively, and, in 16 pts with WBC>13G/l, 9 had at least 2 GFM poor prognostic factors).19 pts still had palpable SPM before allo-SCT. The donor was an HLA-identical, unrelated and haploidentical sibling in 41/31/1 cases respectively. 30pts (41%) received a myeloablative conditioning (MAC) regimen, while 43pts (59%) received reduced-intensity conditioning (RIC). With a median follow-up of 23 mo (1–145), grade 0–1 acute GVHD developed in 23 pts, grade 2–4 in 21 pts. Chronic GVHD was present in 25 pts (35%) (limited:15, extensive: 10; cum incidence: 37% at 3 yrs).The 2- and 3-yr OS were 42% and 32%, respectively. 45 patients had died (23 NRM, 19 disease progression, and 3 unrelated). The 3-yr cum incidence of NRM was 36%. The 3-yr relapse-free survival was 30%. OS was not influenced by the disease status at allo-SCT, including CMML1 vs CMML2, IPSS score (WBC<13G/l) and GFM score (WBC>13G/L), the number of prior treatments, HLA matching, cGVHD. However, palpable SPM at diagnosis was a negative prognostic factor for OS (2-yr OS: 57% vs.15%, p=0.009). 3-yr OS was 33% after MAC conditioning vs 49% after RIC conditioning (p=0.17). In multivariate analysis, the strongest prognostic factor for OS was palpable SPM at diagnosis (HR=2.79 95% CI: 1.38–5.68; p=0.005).
Allo-SCT is a valid treatment option for CMML patients eligible to this treatment. Palpable SPM at diagnosis was the only independent negative prognostic factor. Most pts were however treated before the advent of hypomethylating agents. The use of RIC regimens combined to those agents (and possibly to other novel agents) prior and after allo-SCT may further improve outcome.
Park:Amgen: Honoraria; Celgene: Honoraria; Janssen: Honoraria. Yakoub-Agha:celgene: Honoraria, Research Funding. Fenaux:Celgene: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Janssen Cilag: Honoraria, Research Funding; Roche: Honoraria, Research Funding; Amgen: Honoraria, Research Funding; Glaxo Smith Kline: Honoraria, Research Funding; Merck: Honoraria, Research Funding; Cephalon: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal