Abstract
Abstract 3664
Positron Emission Tomography scans performed during chemotherapy (Interim-PET) have been used prognostically in patients with Diffuse Large B-cell Lymphoma (DLBCL) and as a tool in response-adapted therapy trials. However, evidence on the predictive role of interim-PET in DLBCL has been limited by study heterogeneity in lymphoma subtypes and treatment regimens. Although earlier studies reported positive interim-PET predicted poorer outcome, a systematic review (Terasawa et al. J Clin Oncol 2009; 27(11):1906–14) could not draw reliable conclusions due to heterogeneity. Recent studies, which maintained a homogeneous patient group with regards to lymphoma subtype (DLBCL) and treatment (Rituximab-CHOP), showed conflicting results (Vitolo et al, Blood 2010; 116: Abs. 2819. Yang et al, Blood 2010; 116: 1799. Gonzalez-Barca et al Blood 2010; 116: Abs. 2793.)
To evaluate the prognostic value of interim-PET in DLBCL patients receiving R-CHOP, without the confounding effect of therapy change based on interim-PET result. We seek to improve our prognostic ability by combining the International Prognostic Index (IPI) with Interim-PET results.
We reviewed retrospectively consecutive DLBCL patients treated with R-CHOP as frontline therapy from 2005 to 2010 at a single institution. Interim-PET images were re-examined by a nuclear medicine physician blinded to the IPI and clinical outcomes. The PET results were classified as Negative or Positive, based on qualitative assessment of the relative intensity of FDG uptake of the area of disease compared to the adjacent mediastinal blood pool or aorta/IVC. Interim-PET was categorised as positive if the uptake was more than mildly above the blood pool intensity.
One hundred patients commenced R-CHOP (14 or 21) therapy for DLBCL; 24 patients did not receive interim-PET for logistics reasons and were excluded. Progression free survival (PFS) and overall survival (OS) were analysed by the Cox proportional hazards model and prognostic accuracy was assessed using Harrell's C statistics.
In 76 patients analysed, the median age was 61 years (range 16–87); 59% were males. The IPI distribution was: IPI 0 (n=10), 1 (19), 2 (21), 3 (13), 4 (12), 5 (1). The median time of the interim-PET was after cycle 3.
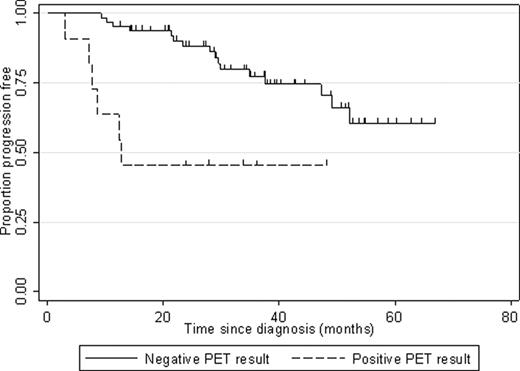
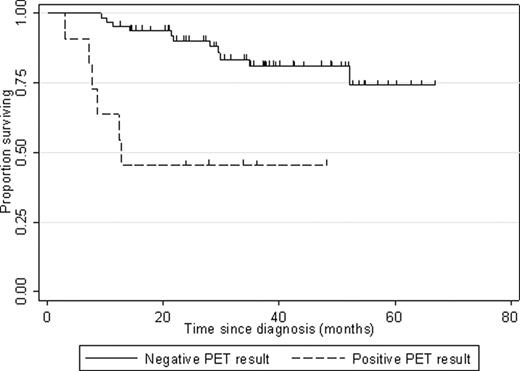
Eleven patients (14%) were positive and 65 patients (86%) were negative at Interim-PET. With a median follow-up of 32.5 months, 2-year OS and 2-year PFS (figures 1 and 2) were 70.8% and 60.0% respectively in the PET-negative group, 36.4% and 36.4% for the PET-positive group (log-rank p-value 0.003 for OS, 0.011 for PFS).
Kaplan-Meier curves for progression-free survival by result of interim PET (p=0.011)
Kaplan-Meier curves for progression-free survival by result of interim PET (p=0.011)
Kaplan-Meier curves for overall survival by result of interim PET (p=0.003)
Correlation analysis showed that the IPI and Interim-PET were minimally associated (rho=0.0873) and were both independent prognostic factors for survival. Cox regression analysis showed that interim PET and IPI were both significant indicators of PFS (p < 0.001 and p=0.002 respectively).
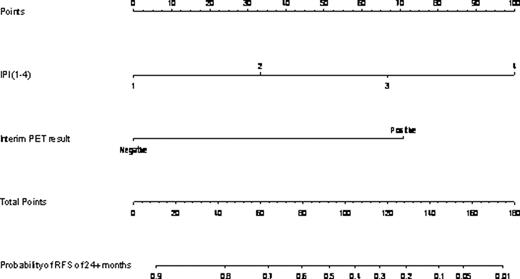
The PET result makes a significant contribution to prognostication if IPI is greater than 2 (p<0.0001) and we found the contribution to vary by IPI when the score was greater than 2 (data not shown). In isolation, the prognostic accuracy of a negative PET result is poor (C = 0.63) as it is for IPI (C = 0.75), but when the two indicators are combined the predictive accuracy is improved (C = 0.81). A nomogram utilising the IPI and interim-PET results in the prediction of the 24 month relapse-free survival was created (Figure 3).
Nomogram for 24 month Relapse-free survival based on IPI and interim PET result
In our hands, IPI and PET provide independent prognostic information; we found interim PET to have a negative predictive value that varies according to the IPI at diagnosis. By combining the two, a more powerful predictive model may be created as a nomogram. This should be readily testable in larger patient populations where PET data is available, and then ideally prospectively in randomised clinical trials.
Example of using the Sir Charles Gairdner Hospital Nomogram: a patient with an IPI of 2 will receive a score of 33; if their interim-PET result is positive, this will produce a score of 70, resulting in a total score of 103. On the lower 2 panels, a total of 103 points is estimated to give rise to a 40% probability of Relapse-free survival at 24 months.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal