Abstract
Abstract 3648
Hodgkin Lymphoma (HL) is generally associated with young age and high cure rates, but inferior outcomes are seen in the 15–20% of patients (pts) aged ≥60 at diagnosis. Failure free survival rates (FFS) are reported at 30–50% for older pts vs 70–85% for younger pts. Reasons for inferior outcomes include ageism, comorbidity, more aggressive biology, reduced dose intensity and excess toxicity; hence, standard ABVD is difficult to tolerate, and more aggressive regimens like BEACOPP excessively toxic. The International Prognostic Score (IPS), used to predict outcomes in advanced (adv) HL, has not been specifically examined in pts >60 years. We sought to characterize the risk factors, tolerance of treatment and outcomes among elderly HL pts at our institution.
We reviewed records for pts ≥ 60 years old with a diagnosis of HL seen at MSKCC between January 1994 and December 2008. Data was extracted regarding demographics, prognostic features, treatment, and outcomes including toxicity, overall survival (OS) and disease specific survival (DSS).
238 pts were identified of whom 105 were excluded from analysis, primarily due to second-opinion only/incomplete records (n=58), age <60 years at diagnosis (n=38), and diagnosis other than HL (n=6), leaving 133 pts for analysis. Characteristics of this group are described in table 1.
| . | N . | % (range) . | . | N . | % (range) . |
|---|---|---|---|---|---|
| Median Age (years) | 68 | (60–88) | B symptoms | 52 | 39% |
| Male | 68 | 51% | Spleen involvement | 16 | 12% |
| Histology | Bulk (node ≥10 cm) | 4 | 3% | ||
| Nodular sclerosis | 66 | 50% | EBV | ||
| Classic, not specified | 28 | 21% | negative | 41 | 31% |
| Mixed cellularity | 27 | 20% | positive | 25 | 19% |
| Lymphocyte rich | 3 | 2% | unknown | 67 | 50% |
| Lymphocyte depleted | 1 | 1% | Comorbid malignancy | ||
| Lymphocyte Predominant | 8 | 6% | Non-Hodgkin Lymphoma | 14 | 10% |
| Stage: | Solid tumor | 23 | 10% | ||
| I | 22 | 17% | Moderate or Severe Comorbidity | 101 | 76% |
| II | 34 | 26% | IPS Risk Factors | ||
| III | 38 | 29% | low albumin | 48/117 | 41% |
| IV | 39 | 29% | WBC >15k | 11/121 | 9% |
| Early (I–II) | 51 | 38% | Hgb <12.5 | 33/121 | 27% |
| Advanced (IIX–IV) | 82 | 62% | <8% lymphs OR ALC <0.6 | 24/115 | 18% |
| . | N . | % (range) . | . | N . | % (range) . |
|---|---|---|---|---|---|
| Median Age (years) | 68 | (60–88) | B symptoms | 52 | 39% |
| Male | 68 | 51% | Spleen involvement | 16 | 12% |
| Histology | Bulk (node ≥10 cm) | 4 | 3% | ||
| Nodular sclerosis | 66 | 50% | EBV | ||
| Classic, not specified | 28 | 21% | negative | 41 | 31% |
| Mixed cellularity | 27 | 20% | positive | 25 | 19% |
| Lymphocyte rich | 3 | 2% | unknown | 67 | 50% |
| Lymphocyte depleted | 1 | 1% | Comorbid malignancy | ||
| Lymphocyte Predominant | 8 | 6% | Non-Hodgkin Lymphoma | 14 | 10% |
| Stage: | Solid tumor | 23 | 10% | ||
| I | 22 | 17% | Moderate or Severe Comorbidity | 101 | 76% |
| II | 34 | 26% | IPS Risk Factors | ||
| III | 38 | 29% | low albumin | 48/117 | 41% |
| IV | 39 | 29% | WBC >15k | 11/121 | 9% |
| Early (I–II) | 51 | 38% | Hgb <12.5 | 33/121 | 27% |
| Advanced (IIX–IV) | 82 | 62% | <8% lymphs OR ALC <0.6 | 24/115 | 18% |
110 pts (83%) were treated with curative intent chemotherapy; the most common regimen used was ABVD in 71 pts (66%), followed by Stanford V in 13 pts (12%) and MOPP-like regimens in 6 (5%). 52 pts (35 early, 17 adv) received radiation. Cause of death was HL in 20 (33.3%), unknown in 19 (31.6%), other malignancy in 14 (23%), toxicity in 7 (12%).
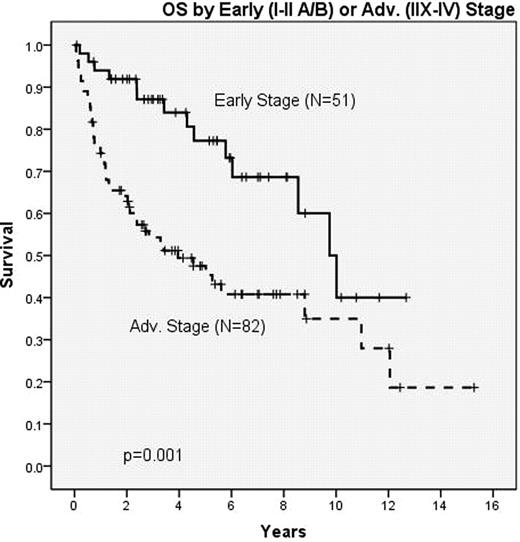
Median OS and DSS, respectively: for all pts was 8.6 and 9.8 years; for early stage both OS and DSS 10.0 years and for adv stage 4.0 and 8.8 years. Median follow-up for surviving pts was 4.5 years, at which time Kaplan-Meier (KM) estimates of OS for all pts/early stage/adv stage are 64%/ 81%/49% respectively (figure 1, 2). DSS for all pts/early stage/adv stage are 69% / 90% / 58%.
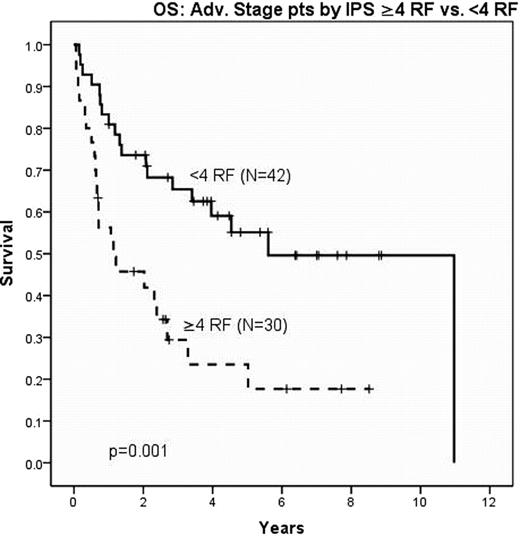
Complete data was present for all IPS variables in 72 of 82 adv stage pts. Thirty (41.7%) pts had ≥4 IPS risk factors and significantly inferior OS and DSS of 24% and 35%, respectively compared with 59% and 66% with <4 IPS risk factors. Median OS and DSS for the high risk group were both 1.1 years; in low risk pts they were 5.6 years (OS) (Figure 3) and 11 years (DSS). EBV status, comorbidity and any dose delays >7 days or >14 days did not predict outcome. Interim PET scan was performed on 33 pts, of whom 22 were adv stage. Nine of 22 were performed after the 2nd cycle and 13 after the 4th. There was a trend toward inferior survival in 8 pts with positive interim PET compared to 14 with negative interim PET (p=0.077).
Elderly HL pts treated at MSKCC frequently had adverse baseline risk factors including mixed cellularity histology, adv. stage, high comorbidity, and IPS≥4 at presentation; despite this, curative intent therapy was given in 83% of pts and is associated with outcomes comparable to reported clinical trials in elderly HL. The IPS is predictive of outcome in adv stage elderly HL pts, with IPS≥4 associated with worse outcomes; Interim PET scans also trended to predict outcome in this population. Our analysis supports the need for development of novel treatment paradigms in this patient population.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal