Abstract
Abstract 3590
Treatment decisions for early re-induction of patients with de novo acute myeloid leukemia (AML) based on sub-optimal cytoreduction as seen on day 14 bone marrow (BM) biopsy is laden with controversy. The aim of our review was to correlate results of the day 14 BM biopsy to overall outcomes of induction therapy.
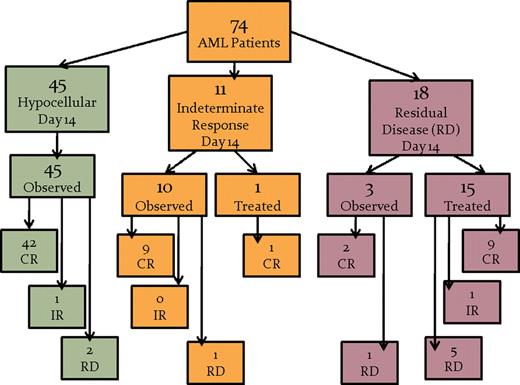
Between November 1995 and July 2008, medical records for patients treated for de novo AML were retrospectively reviewed for the purpose of evaluating treatment decisions and outcomes based on day 14 BM biopsies. Of all patients treated during that period, 100 patients were categorized as de novo AML, and were treated with standard induction chemotherapy. Seventy-four (n=74) of these patients had paired BM biopsy reports. Response to therapy was based purely on morphology noted by the pathologist on the day 14 BM in this analysis, with indeterminate response (IR) defined as a hypocellular marrow (HM) with moderate increase in blasts above 5% in which the reviewing pathologist could not rule out the possibility of persistent leukemia. Residual disease (RD) was defined by the reviewing pathologist as grossly elevated percentages of abnormal populations of persistent blasts by morphology alone definitively consistent with residual disease (i.e. no flow cytometric or molecular adjuncts). Otherwise, the patients were classified as appropriate response with a HM and less than 5% blasts with no evidence of residual leukemia.
Day 14 BM biopsies of the 74 patients (median age = 42 years, range 18 to 77) undergoing standard induction chemotherapy revealed that 45 patients (61%) had a HM with less than 5% blasts. Eleven patient's (15%) BM biopsies were classified as IR. Eighteen patients (24%) had morphologically definitive RD. In all, 29 patients (39%) had a sub-optimal response (SOR) to induction chemotherapy (IR+RD=SOR). The 45 patients with HM and low blast percentage were observed until count recovery as is the usual practice. However, 16 of 29 patients with SOR received re-induction chemotherapy (1 IR and 15 RD) of which 10 patients attained a morphologic CR (9 RD and 1 IR). The 13 remaining patients (3 RD and 10 IR) were observed without any re-induction therapy, and re-evaluated with a follow-up BM biopsy between days 21 and 42 of initial induction. Interestingly, 11 of these 13 patients had a morphologic CR on follow-up biopsy, including 2 of 3 patients initially categorized as RD. Analysis of the paired results from nadir to recovery for the 58 observed patients in this cohort revealed a positive predictive value (PPV) and negative predictive value (NPV) for the day 14 BM biopsy review of 15% and 93% respectively.
Our data suggests that those patients with an IR on day 14 may not necessarily require re-induction chemotherapy, and may actually benefit from careful observation by avoiding the risks of reinduction and prolonged cytopenias. Thus, while the day14 BM is an important tool for the evaluation of response in AML patients undergoing induction therapy, it is not always a reliable test for residual leukemic burden, as illustrated by its low PPV. As such, future treatment decisions should be weighted by, but not based solely on this parameter. Our future plans are to evaluate this question prospectively in a larger cohort of de novo AML patients receiving induction therapy with centralized pathologic review, and also to look at the effect of cytogenetic and molecular mutation analysis at day 14 on treatment decision making and outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal