Abstract
Abstract 3588
Leukemia is a common hematologic malignancy for which the etiology remains largely unclear. The epidemiological data regarding the link between overweight and obesity, as defined by body mass index (BMI), and the risk of developing leukemia has revealed conflicting results. The main objective of this meta-analysis is to evaluate the potential relationship that overweight and obesity may have in the development of leukemia in adults. A secondary objective was to evaluate the risk of separate leukemia subtypes such as acute myeloid leukemia (AML), acute lymphoblastic leukemia (ALL), chronic myeloid leukemia (CML) and chronic lymphocytic leukemia (CLL).
A MEDLINE search from January 1950 to December 2010 was undertaken using: (obesity OR “body mass index” OR BMI OR overweight) AND (leukemia OR lymphoma OR myeloma). Only prospective cohort studies reporting on the incidence of leukemia were included. Retrospective case-control and cross-sectional studies were excluded. Meta-analyses were performed for leukemia in general and leukemia subtypes. The outcome was calculated as relative risk (RR). Overweight was defined as BMI 25–29.9 kg/m2 and obesity as BMI ≥30 kg/m2, according to the WHO criteria. The quality of the studies was determined by the Newcastle-Ottawa scale (NOS). The random effects model (REM) was used to calculate the combined outcome. Heterogeneity was assessed by the I2 statistic. Publication bias was assessed by the trim-and-fill analysis. Meta-regression analyses were performed to evaluate the association between BMI, as a continuous variable, and the incidence of leukemia in general as well as BMI and leukemia subtypes. Literature search, data gathering and quality assessment were performed independently by at least 2 of the investigators. All graphs and calculations were obtained using Comprehensive Meta-Analysis version 2 (Biostat, Englewood, NJ).
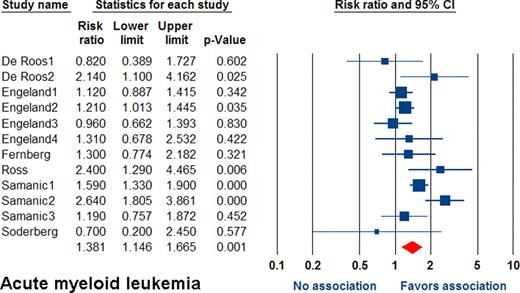
From 758 returns, 19 prospective cohort studies evaluating the association between incidence of leukemia and BMI were identified. All the studies were of high quality (NOS >7 points). When pooling all studies, the RR was 1.14 (95% CI 1.07–1.22; p<0.001). Overweight patients had a RR of 1.11 (95% CI 1.06–1.17; p<0.001), and obese patients had a RR of 1.19 (95% CI 1.09–1.31; p<0.001). Meta-regression showed linear association between BMI and leukemia (p<0.001). For AML, the overall RR was 1.24 (95% 1.10–1.41; p=0.001). Overweight patients had RR of 1.08 (95% CI 0.97–1.20; p=0.18). Obese patients had RR of 1.38 (95% CI 1.15–1.67; p=0.001; Figure). Meta-regression showed a statistically significant linear association between BMI and incidence of AML (p<0.001). For ALL, the overall RR was 1.48 (95% CI 1.20–1.80; p<0.001). Overweight patients had RR of 1.36 (95% CI 1.06–1.76; p=0.02). Obese patients had RR of 1.62 (95% CI 1.13–2.32; p=0.009). Meta-regression showed no association between BMI and incidence of ALL (p=0.25). For CML, the RR was 1.20 (95% CI 1.02–1.41; p=0.03). Overweight and obese patients had RR of 1.05 (95% CI 0.74–1.49; p=0.79) and 1.27 (95% CI 1.10–1.46; p=0.001), respectively. Meta-regression showed no association between BMI and CML (p=0.15). For CLL, the overall RR was 1.13 (95% CI 1.07–1.19; p<0.001). Overweight and obese patients had RR of 1.09 (95% CI 1.03–1.16; p=0.003) and 1.17 (95% CI 1.09–1.25; p<0.001). Meta-regression showed a trend towards a linear association between BMI and incidence of CLL (p=0.06).
Obesity, but not overweight, is associated with a mild-to-moderate increased risk of leukemia in general (19%) and for all leukemia subtypes (AML 38%, ALL 62%, CML 27% and CLL 17%). Additionally, meta-regression analyses showed a statistically significant linear association between increasing BMI and general incidence of leukemia in addition to incidence of AML.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal