Abstract
Abstract 3367
Asian populations are diverse with respect to genetics, healthcare, and living circumstances. Although immune responses to erythrocyte antigens have been exhaustively characterized in various American and European populations, comparable information from Asia is lacking. Collaborative international investigations have the potential to improve transfusion and transplantation outcomes, and also advance anthropological understanding of human evolution and migration. We therefore started a comprehensive survey of alloantibodies (Abs) to erythrocyte antigens in patients from Asian countries. Here we report similaries and differences among a large number of patients in Korea and Japan.
Twenty-one institutes from Korea and 38 from Japan participated in this study of alloantibodies to erythrocyte antigens. We investigated the number of blood grouping tests, cross matching tests, and erythrocyte irregular Ab analyses as well as institutional details such as the total number of beds, operations and transfusions performed. We also investigated methods employed for screening and identifying irregular Abs. Furthermore, we compared the frequencies of irregular Abs to D, C,c, E, e, f, Ce, P1, M, N, S, s, Mia, Lea, Leb, Jka, Jkb, Jk3, Fya, Fyb,K, k, Kpa, Kpb, Jsa, Jsb, Dia, Dib, Lua, Lub, Xga and H between Korea and Japan. The total number of independent cases included more than 1,135,000 patients. If a case was analyzed multiple times, it was counted once. Multiple antibodies in the same patient were separately summarized. We compared the frequencies of irregular Abs on the basis of gender, pregnancy, and transfusion history.
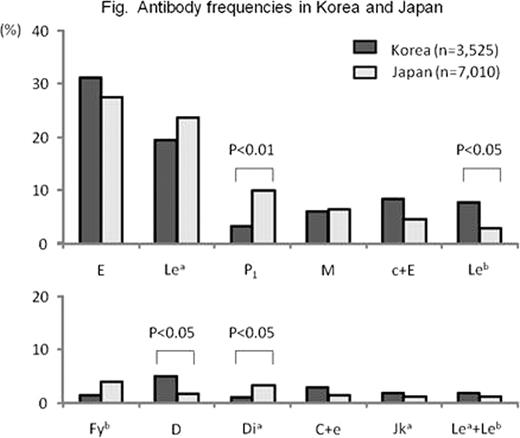
Different methods used at different institutions did not cause statistically significant differences in results. Antibodies were detected in 10,535 patients totally, including 3,525 in Korea and 7,010 in Japan. The female to male ratios were 1.53 and 1.39, respectively. Antibody frequencies are shown in the figure. Anti-P1 and anti-Dia Abs were observed in 3.4% and 0.9% of Korean patients, respectively, versus 10.4% and 3.4% of Japanese patients. These differences were statistically significant between the two countries (p<0.01 and p<0.05, respectively). Anti-D and anti-Leb Abs were observed in 5.1% and 7.8% of Korean patients, respectively, versus 1.6% and 2.9% of Japanese patients. These differences were statistically significant between the two countries (p<0.05 and p<0.05, respectively). Anti-Mia, frequently detected in Thailand (49.3%), Hong Kong (45.4%) and Malaysia (7.0%) in other studies, was not observed in either Korea or Japan. Anti-D was more frequently detected in females (p<0.01), but varies between countries as follows; 1.7/7.2 (male/female, %) in Korea and 0.8 /2.2 in Japan. It was 8.3 and 2.3 times more frequently observed in pregnant patients, (p<0.01 and p<0.05, respectively), but did not change in patients who had received blood transfusion. Anti-E was 1.4 and 1.7 times more frequently detected in patients who had received blood transfusion in Korea and Japan, respectively. Anti-Jka and -C were 1.9 and 8.2 times more likely in patients who had received blood transfusion in either country. Comparing Korea and Japan, Anti-c+E was 2.4 and 3.0 times and anti-C+e was 2.8 and 2.7 times more frequently observed, respectively.
Takeshita:Takeda: Research Funding; Novaltis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal