Abstract
Abstract 3181
Cardiac failure is the leading cause of death in patients with thalassaemia major. However, the introduction of new monitoring techniques, such as cardiac iron Magnetic Resonance Imaging (MRI), may lead to the improvement of patient care and prolong survival. Although the impact of cardiac siderosis in patients with thalassaemia major has been extensively studied, further examination of the effect of specific iron chelators such as deferasirox are important in the development of treatment protocols, while the clinical consequences of cardiac iron accumulation in patients with myelodysplastic syndromes (MDS) is still controversial.
The primary objective of this study is to investigate the effect of single agent deferasirox on cardiac iron levels and cardiac function, in a cohort of patients receiving regular red blood cell transfusions.
Patients with transfusional siderosis were enrolled in this study and received deferasirox for 53 weeks. Doses up to 40 mg/kg/day were allowed according to transfusional requirement, response to chelation therapy and safety markers. Cardiac siderosis (cardiac T2* measured by linear fitting to the decay of logarithmic magnetic resonance signal) and left ventricular ejection fraction (LVEF) were measured at baseline and at 53 weeks. The sample size was originally calculated based on the standard deviation (SD) of the change in log(T2*) (0.47), according to previously published reports. A planned sample size reassessment as per protocol was undertaken when 42 patients had follow-up data. For the sample size reassessment, log(T2*) was calculated for each result and the change in log(T2*) estimated for each patient. Results from the interim sample size reassessment and the analysis of cardiac iron and function are described below.
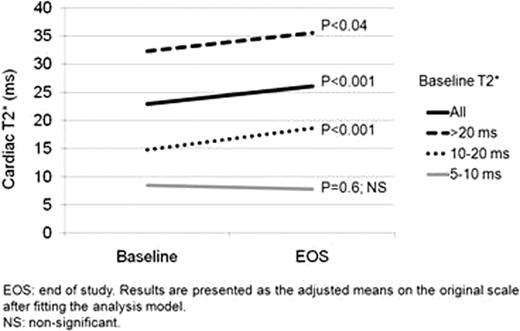
Results were available for 36 patients with haemoglobinopathies (mainly represented by thalassaemia major), 5 patients with MDS and one post-bone marrow transplant patient. The SD observed for change in log(T2*) with the current data was 0.26 (original assumption 0.47). Assuming the SD for the final data does not increase above 0.34 the current cohort should be sufficient to detect a change in log(T2*) of the pre-specified 0.14. Safety assessments were consistent with previous studies on deferasirox. An overall increase in cardiac T2* from 23.0 to 26.1 ms was observed (p<0.001). Further analysis was performed based on the T2* baseline values: 5–10 ms, no significant change (n=6; 8.5 to 7.9 ms; p=0.6; non-significant); 10–20 ms, improvement of 26% (n=8; from 14.8 to 18.7 ms; p=0.001); >20 ms, increase of 10% (n=28; 32.3 to 35.6 ms; p=0.04). Overall, an increase in LVEF of 2.1% was observed, just below statistical significance (from 60.9% to 63.0%, p=0.076). The largest increase in LVEF was observed in patients with moderate cardiac siderosis (baseline T2* 10–20 ms; statistically significant increase in LVEF of 5.7%, from 56.8% to 62.5%, p=0.045). Descriptive preliminary analyses of the MDS subgroup showed that all 5 patients had baseline cardiac T2* >20 ms (median 32 ms; range: 29.7 to 34 ms). Similarly to the overall patient pool, deferasirox induced a 12% increase in cardiac T2* although not statistically significant (32.2 to 35.9 ms, p=0.13). In this subgroup of MDS patients, a statistically significant increase in LVEF was also observed (56.4% to 63.6%, p=0.04). Results on liver iron concentration will also be presented.
The interim results from this study showed for the first time that once-daily deferasirox induced a simultaneous and statistically significant increase in both cardiac T2* levels and cardiac function in patients with moderate cardiac siderosis. Although the small number of patients in the MDS subgroup had cardiac T2* levels above 20 ms, chelation therapy induced an increase in LVEF in all 5 patients enrolled to date. Taken together, these results also confirm previous reports showing that single agent deferasirox is an effective therapy for maintenance and reduction of cardiac iron levels, especially for patients with cardiac T2* >10 ms. Recruitment has been halted based on the recommendations of the interim sample size re-estimation in consultation with the Data Monitoring Committee. Six patients are ongoing, and will be included in the final analysis of the study.
Ho:Novartis: Honoraria, Invited speaker, Membership on an entity's Board of Directors or advisory committees. Tay:Novartis: Membership on an entity's Board of Directors or advisory committees. Teo:Novartis: Research Funding. Marlton:Novartis: Membership on an entity's Board of Directors or advisory committees. Grigg:Novartis: Invited speaker, Membership on an entity's Board of Directors or advisory committees. Pierre:Resonance Health: Consultancy, Equity Ownership, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Consultancy, Research Funding, Speakers Bureau. Brown:Novartis: Consultancy, Invited speaker. Gervasio:Novartis: Employment. Bowden:Novartis: Honoraria, Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal