Abstract
Abstract 3105
relapse after ASCT remains the most important cause of treatment failure among high-risk lymphomas. In order to improve outcome, allogeneic hematopoietic stem cell transplantation (AlloSCT) is used to exploit graft-versus-lymphoma (GVL) effect; on the other hand, feasibility of AlloSCT is limited by the high risk of infections and graft-versus-host disease (GvHD), accounting for transplant-related mortality (TRM) up to 40% in some circumstances.
we retrospectively analyzed data on 34 high-risk NHL patients who underwent ASCT followed closely by reduced-intensity AlloSCT (“tandem auto-allo”) from January 2002 to November 2010. The tandem transplantation decision relied on the high-risk disease, needing some consolidation therapy after ASCT, and on the hypothesis of a high GVL effect when a significant cytoreduction occurred after AlloSCT. The search for an allogeneic donor was started at the beginning of salvage regimen. Preparative regimen for reduced-intensity AlloSCT was an association of fludarabine-busulfan-ATG or fludarabine-cyclophosphamide with our without thiotepa. In one patient conditioning was BEAM regimen. GvHD prophylaxis included cyclosporine alone or in combination with methotrexate.
median patients' age at AlloSCT was 47 (27–68); hystotypes were as follows: diffuse large B-cell n= 5, follicular n= 14, transformed follicular n= 4, mantle-cell n= 5, lymphoplasmocytic lymphoma n=1, anaplastic large T-cell n= 2, peripheral T-cell n= 3. Donor were HLA-identical sibling (n= 29) or 10/10-matched unrelated (n=5). Peripheral stem cell was used in all patients but one. Median interval between ASCT and AlloSCT was 76 days (36–197). Median prior therapeutic lines before tandem transplantation were 2 (0–4). Overall, 16 patients were in complete remission, 13 were in partial remission and five were in progressive disease at time of AlloSCT.
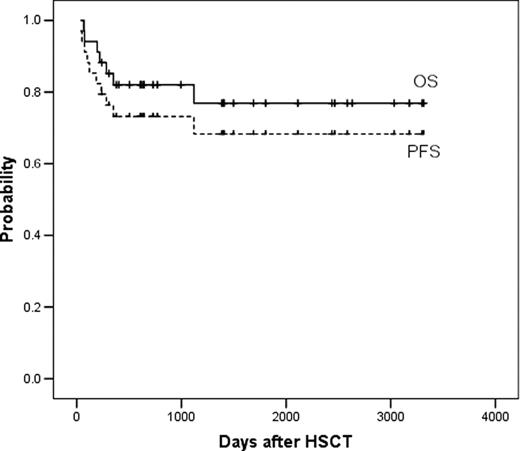
Successful allogeneic engraftment occurred in all patients. At a median follow-up of 46 (8–108) months since AlloSCT, 5-year overall survival (OS) is 77% (61–93) and progression-free survival (PFS) is 68% (51–85) (figure 1). Disease relapse or progression occurred in six patients (18%), 100-day TRM was 0%, overall TRM rate was 9%. Causes of TRM were: infection in two patients and severe extensive chronic GvHD in one patient. Ten patients developed grade >=2 acute GvHD and fifteen patients chronic GvHD, respectively.
tandem transplantation is feasible in relapsed or refractory NHL patients having a HLA-identical allogeneic stem cell donor, with 0% early TRM and 9% overall TRM rate. This tandem approach, i.e. disease debulking by salvage therapy and ASCT followed by allogeneic GVL immunotherapy, could represent a suitable therapeutic option for those patients. This invites promptly starting a donor search in these situations.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal