Abstract
Abstract 3083
More active high-dose regimens are needed for lymphomas and myeloma (MM), where standard BEAM and melphalan offer unsatisfactory results in refractory tumors. Gem has not been adequately explored at high doses despite its favorable pharmacological and toxic profile and activity against lymphomas. We wished to dose-escalate Gem infused at a fixed dose rate (FDR) of 10 mg/m2/min, which optimizes its intracellular activation as compared to its usual short infusions. We combined Gem with BuMel to exploit their synergy based on Gem-mediated inhibition of DNA damage repair.
Pts with refractory Hodgkin's (HL), non-Hodgkgin's lymphoma (NHL) and MM and normal end-organ function were eligible for this dose- and schedule-finding study. Gem was given as a loading dose of 75 mg/m2 followed by FDR infusion on 3 different schedules: daily (d-8 to d-5 and d-3 to d-2), 3 doses (d-8, d-6 and d-3) and 2 doses (d-8 and d-3). Each Gem dose was immediately followed by the corresponding dose of Bu or Mel. After a test dose on d-10, Bu was given from d-8 to d-5 targeting a daily AUC of 4, 000. Mel was infused at 60 mg/m2/d on d-3 and d-2. PBPC were infused on d0. Pts with CD20+ tumors received rituximab (375 mg/m2) on d+1 and d+8. Gem dose escalation proceeded by prolonging its infusion at FDR from dose level 1 (15-min infusion). Dose limiting toxicities (DLT) were defined as any G4-5 nonhem organ toxicity or G3 skin or mucositis lasting >3 days at peak severity. Dose escalation followed a Bayesian design targeting a 15% DLT probability.
Between 1/07 and 7/11, 130 pts were enrolled (Table 1).
Clinical features.
| . | HL . | NHL . | MM . |
|---|---|---|---|
| N | 79 | 44 | 7 |
| Median age | 30 (18–61) | 53 (26–66) | 56 (47–62) |
| % primary induction failure (PIF)/% refractory relapse | 63%/37% | 45%/55% | 71%/29% |
| Median IPI at relapse/PD | N/A | 3 (1–4) | N/A |
| Median # prior regimens (range) | 2 (2–6) | 3 (1–9) | 3 (2–5) |
| Median # prior relapses/PD (range) | 1 (1–5) | 2 (1–8) | 2 (1–4) |
| Prior Gem | 44% | 14% | 0% |
| Prior xRT | 28% | 24% | 43% |
| PET+ at HDC | 52% | 55% | N/A |
| PD at HDC | 27% | 16% | 57% |
| . | HL . | NHL . | MM . |
|---|---|---|---|
| N | 79 | 44 | 7 |
| Median age | 30 (18–61) | 53 (26–66) | 56 (47–62) |
| % primary induction failure (PIF)/% refractory relapse | 63%/37% | 45%/55% | 71%/29% |
| Median IPI at relapse/PD | N/A | 3 (1–4) | N/A |
| Median # prior regimens (range) | 2 (2–6) | 3 (1–9) | 3 (2–5) |
| Median # prior relapses/PD (range) | 1 (1–5) | 2 (1–8) | 2 (1–4) |
| Prior Gem | 44% | 14% | 0% |
| Prior xRT | 28% | 24% | 43% |
| PET+ at HDC | 52% | 55% | N/A |
| PD at HDC | 27% | 16% | 57% |
The daily and 3-dose Gem schedules showed excessive skin toxicity after enrollment of 2 pts on each. In contrast, the 2-dose schedule was well tolerated, allowing Gem escalation from level 1 to level 9 (270-min infusion, daily dose 2, 775, total dose 5, 550 mg/m2), which was established as the MTD with mucositis approaching the prespecified target DLT probability. Neutrophils and platelets engrafted promptly at median d+10 and +11, respectively. There were 2 treatment-related deaths from MOF (daily schedule) and Pseudomonas pneumonia (level 5 of 2-d schedule). Toxicities of the 2-d schedule were 2G3 and reversible, including mucositis, skin rash, transaminase elevation and hyperbilirubinemia (1 case of VOD) (Table 2). Lung toxicity was minimal, with 1 G2 and 1 G3 pneumonitis and no difference in DLCO pre- and 1-mo post-HDC: median 75% v 77% (P=0.45).
Toxicity profile (2-d schedule).
| . | N . | % DLT . | Mucositis . | Rash . | AST/ALT . | Bilirubin . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | % G2 . | % G3 . | % G2 . | % G3 . | % G2 . | % G3 . | % G2 . | % G3 . |
| Overall | 126 | 7 | 60 | 18 | 17 | 1.6 | 20 | 10 | 10 | 5 |
| Level 9 (MTD) | 25 | 12 | 44 | 44 | 16 | 4 | 8 | 8 | 4 | 8 |
| . | N . | % DLT . | Mucositis . | Rash . | AST/ALT . | Bilirubin . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | % G2 . | % G3 . | % G2 . | % G3 . | % G2 . | % G3 . | % G2 . | % G3 . |
| Overall | 126 | 7 | 60 | 18 | 17 | 1.6 | 20 | 10 | 10 | 5 |
| Level 9 (MTD) | 25 | 12 | 44 | 44 | 16 | 4 | 8 | 8 | 4 | 8 |
Pts who had G3 tox tended to be younger than those who did not (median age 35 v 43, P=0.05), with no differences between both groups in pre-HDC values of C-reactive protein, BNP, ferritin or haptoglobin. Planned post-HDC xRT was given to 24 pts (21 HL, 3 NHL) at a median 1 mo post-HDC and was well tolerated.
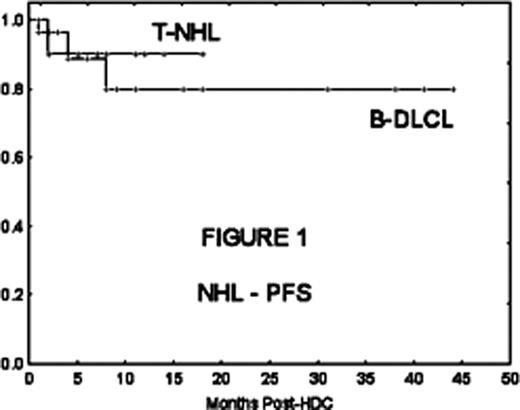
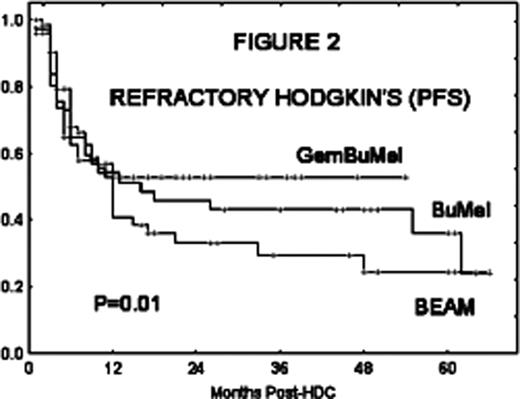
Activity and patient outcomes at median follow-up of 16 mo (1–54) are shown on Table 3 and Figs 1 and 2:
Efficacy.
| . | . | N . | % responses . | %CR . | % PFS . | % OS . |
|---|---|---|---|---|---|---|
| HL | 79 | 87% | 63% | 63% | 88% | |
| NHL | B-LCL | 29 | 100% | 69% | 89% | 89% |
| T-NHL | 10 | 66% | 66% | 70% | 70% | |
| Burkitt's | 4 | 100% | 75% | 25% | 25% | |
| MM | 7 | 86% | 43% | 43% | 43% |
| . | . | N . | % responses . | %CR . | % PFS . | % OS . |
|---|---|---|---|---|---|---|
| HL | 79 | 87% | 63% | 63% | 88% | |
| NHL | B-LCL | 29 | 100% | 69% | 89% | 89% |
| T-NHL | 10 | 66% | 66% | 70% | 70% | |
| Burkitt's | 4 | 100% | 75% | 25% | 25% | |
| MM | 7 | 86% | 43% | 43% | 43% |
Further, we compared the HL subgroup with all other refractory HL pts treated during the same period at MDACC who met eligibility criteria for the GemBuMel trial but either received BEAM off protocol (N= 83) or were enrolled in a separate trial of BuMel (N=38). They all met ≥1 of the following protocol-specified criteria of refractory disease: PIF, CR1 <6 mo, >1 relapse/PD or PET+ at HDC. The 3 groups had comparable age, CR1 length, prior xRT, % relapse within a prior xRT field, or % B symptoms at relapse/PD. However, the GemBuMel group had significantly higher % PIF, # prior regimens, % PET + tumors and % PD at HDC. Despite their worse prognostic features GemBuMel pts had improved EFS (P=0.01) and OS (P=0.01) than those receiving BEAM or BuMel (Fig 2).
GemBuMel is a new safe and highly active HDC regimen for refractory HL and NHL, which warrants its further study in disease-specific trials.
Nieto:Otsuka Pharmaceuticals: Research Funding. Off Label Use: Gemcitabine, busulfan and melphalan: Use at high doses for lymphomas and myeloma.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal