Abstract
Abstract 304
Bendamustine is a bifunctional alkylating agent that is approved for the treatment of chronic lymphocytic leukemia and indolent non-Hodgkin's lymphoma. This first multicenter, phase I/II trial investigated the combination of bendamustine, lenalidomide and dexamethasone (BLD) as a potentially effective treatment option for multiple myeloma (MM) patients, particularly for those with pre-existing or bortezomib-induced neuropathy. Our primary objective was to determine the maximum tolerated dose (MTD) and safety profile of bendamustine and lenalidomide when administered with dexamethasone for patients with relapsed or refractory MM.
We conducted an open-label, dose escalation study (Table 1). Patients were enrolled from June 2008 through February 2011. Eligible patients were aged ≥ 18 years with confirmed, measurable stage II or III MM that was refractory to or progressed after 1 or more prior therapies including lenalidomide. Patients were assigned to their dose levels in a classical 3+3 cohort design. Phase I was to assess the safety and to establish the MTD of the combination treatment. The phase II portion of the study was to assess the overall response rate (ORR) at the MTD. Intravenous bendamustine was given on days 1 and 2, oral lenalidomide on days 1–21, and oral dexamethasone on days 1, 8, 15, and 22 of the 28-day cycle. Treatment was given until plateau of best response as determined by the International Myeloma Working Group uniform response criteria for a maximum of 8 cycles. The study doses were escalated through 3 levels, in a 3+3 dose escalation scheme. The MTD was defined as the dose level at which ≤1 of 6 patients experienced dose-limiting toxicity (DLT) during the first cycle of therapy when the next higher dose level was associated with DLTs in ≥ 2 patients. Primary endpoint was the MTD. After determining the MTD, up to 12 additional patients were enrolled in an MTD expansion arm to better evaluate toxicity and clinical activity. Secondary endpoints included preliminary efficacy, as evidenced by objective response, time to disease progression, and overall survival.
| Dose level . | Bendamustine, mg/m2 . | Lenalidomide, mg . | Dexamethasone, mg . |
|---|---|---|---|
| 1 | 75 | 5 | 40 |
| 2 | 75 | 10 | 40 |
| 3 | 100 | 10 | 40 |
| Dose level . | Bendamustine, mg/m2 . | Lenalidomide, mg . | Dexamethasone, mg . |
|---|---|---|---|
| 1 | 75 | 5 | 40 |
| 2 | 75 | 10 | 40 |
| 3 | 100 | 10 | 40 |
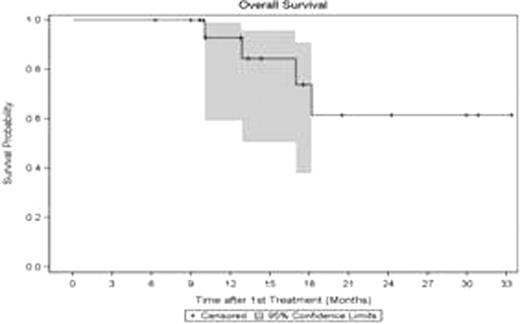
36 patients with a median age of 63 years (range 38 to 80) were enrolled. The median number of prior therapies was 3 with a range of from 2–9; 79% of the patients had prior lenalidomide, 48% had prior thalidomide, and 34% had both. 69% of the patients had a prior autologous stem cell transplant. The MTD was 75 mg/m2 for bendamustine and 10 mg for lenalidomide. DLTs included at dose level 2: 1 grade 4 neutropenia; at dose level 3: 2 grade 4 neutropenias and 1 delayed platelet recovery from grade 3 thrombocytopenia. 25 received at least 2 cycles and were included into the response assessment. A partial response or better was observed in 52% (n=13) of the patients, including 24% (n=6) VGPR. MR was observed in 24% (n=6), SD 16% (n=4), and PD 8% (n=2). BLD induced fast responses with a time to best response of 1.6 months (range 0.7–7.4). The response was independent of prior exposure to lenalidomide evidenced by the fact that 84% of patients with VGPR/PR had prior treatment with lenalidomide. The median follow up for patients at risk of progression is 8 months (range 4–13). The estimated median progression free survival (PFS) is 4.4 months (95% CI (3.4, 9.2). 4 patients have died and the median follow up for patients who are still alive is 13 months (range 6–33). The median OS survival has not been reached yet. We did not observe any unanticipated DLTs. The only grade 4 adverse events for all patients for all cycles included 24.1% neutropenia and 7% thrombocytopenia. No infection was associated with the neutropenia and all AE resolved successfully.
This is the first phase I/II trial testing bendamustine, lenalidomide and dexamethasone in combination for relapsed and refractory MM. This regimen is safe and well tolerated even in older patients up to 80 years. Based on the mainly myelosuppressive side effects, concomitant treatment with filgastrim is recommended. This regimen induced fast responses and high response rates even in heavily pretreated MM patients. The high responses were also achieved in patients with prior exposure to lenalidomide suggesting that BLD overcomes resistance to lenalidomide and is a highly active regimen.
Lentzsch:Celgene Corp: Consultancy, Research Funding; Onyx: Consultancy; Genzyme: Consultancy; prIME Oncology: Honoraria; Imedex: Honoraria; Clinical Care Options: Honoraria. Burt:Celgene Corp: Honoraria, Speakers Bureau; Cephalon: Honoraria, Speakers Bureau. Roodman:Amgen: Consultancy; Millennium Pharmaceuticals: Consultancy. Agha:Novartis: Consultancy. Zonder:Millennium: Consultancy, Research Funding, Speakers Bureau; Celgene: Speakers Bureau; Medtronics: Honoraria; Amgen: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal