Abstract
Abstract 3003 FN2
FN2
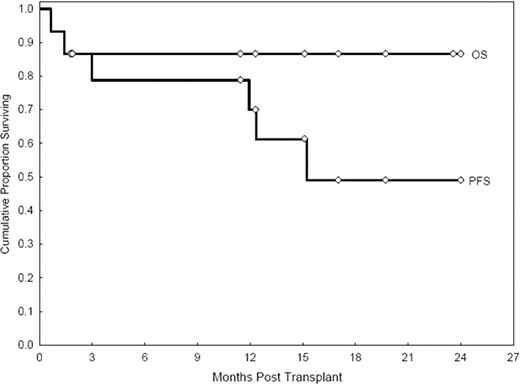
Progressive disease (PD) remains the main cause of treatment failure following RIC allo-SCT in HL (Peggs KS et al, BJH 2008: 143; 468). We elected to explore the feasibility of adding gemcitabine (G), a highly active agent in relapsed/refractory HL (Santoro A et al, JCO 2000 :18; 2615), to our standard fludarabine (F) - melphalan (M) RIC in patients with relapsed and refractory HL undergoing allo-SCT, with the ultimate goal to augment cytoreduction and reduce the incidence of PD. Main G-associated non-hematologic toxicities include pulmonary, skin toxicities and mucositis. Patients and Methods: Between 8/07 and 3/11, fifteen consecutive HL patients (Unique Patient Number/UPNs 1–15) underwent an allo-SCT with the G-FM regimen. They had failed multiple conventional treatments (median prior chemotherapy regimens: 4; range 2–9), radiation therapy (6/15) and a prior auto-SCT (7/15). The median age was 33 years (range 20–46). Disease status at SCT was chemosensitive relapse (n=4), untreated relapse (n=1), induction failure chemosensitive (n=2), complete remission undetermined (CRU1 and CRU2) (n=8). The median time to PD after auto-SCT was 10 months (range 3–19). The donor was an HLA-identical sibling (n=10) or matched unrelated donor (MUD; n=5, with UPN 6 having a 9/10 match). The conditioning regimen was G 800 mg/m sq IV x1 at day -7 (two patients, UPN 6 and UPN 7 received G 1000 mg/m sq IV x2, day -5 and day -2 as part of a dose escalation attempt stopped for excess toxicity), F (32 mg/m sq IV x4, day -5 to day -2), M (70 mg/m sq IV x2, day -3 and day -2; total dose 140 mg/m sq). Thymoglobulin (4 mg/kg IV) was added in MUD allografts. Graft-vs-host disease (GVHD) prophylaxis included tacrolimus and mini-dose methotrexate (5 mg/m sq). Results: Myeloid recovery was prompt, with an absolute neutrophil count (ANC)>500/mcL at day +12 (range 11–20). Median platelet recovery at 20K/mcL was at day +14 (range 9–26). Chimerism studies indicate 100% donor-derived engraftment in 13/13 evaluable patients (100%). Day 100/overall transplant-related mortality (TRM) were 2/15 (13%) and 2/15 (13%), respectively. Acute GVHD (grade II-IV) occurred in 8/14 evaluable patients, chronic GVHD in 7/13 evaluable patients (extensive in 7). Pulmonary toxicity was seen in four patients (26%). Grade 4 pulmonary toxicity was seen in UPN 6. Otherwise it was grade 1–2 (n=3). Cutaneous toxicity (skin rash, responsive to steroid therapy) was seen in five patients (33%: grade 3 n=1; grade 1–2 n=4). Mucositis was seen in nine patients (60%). It was grade 3 (n=1); grade 1–2 (n=8). Other organ toxicities were not seemingly markedly different from the ones seen with FM140 only. Three patients expired (graft rejection n=1, in UPN 6; CMV pneumonia n=1; PD n=1). Twelve patients are alive (ten progression-free, eleven in CR/CRU) with a median follow-up of 18 months (range 2–33). Actuarial rates of overall survival (OS) and progression-free survival (PFS) at 24 months are 87% (95% CI: 56–96) and 49% (95% CI: 18–74), respectively (see Figure). While a formal comparison with our historical experience with the FM140 regimen is clearly not possible, OS and PFS (actuarial estimates) at 24 months were 64% (95% CI: 49–76), and 32% (95% CI: 20–45), respectively (Anderlini et al, Haematol 2008; 93 :257). Conclusions: The addition of G to FM140 is feasible. Pulmonary, cutaneous toxicities, as well as mucositis, while clinically significant, were manageable and did not contribute to mortality in the patients treated with only one G dose. While quite encouraging, these data remain preliminary. The G-FM regimen deserves further study in a larger cohort of patients.
Off Label Use: Gemcitabine, fludarabine and melphalan as part of conditioning regimen for allogeneic stem cell transplantation.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal