Abstract
Abstract  2868
2868
Improvement in renal parameters is fundamental for the assessment of organ response to treatment in immunoglobulin light chain amyloidosis (AL). Renal response, defined as a >50% reduction in proteinuria with <25% decrease in renal function, is associated with superior overall survival (OS); however, a systematic study of the interplay of proteinuria, creatinine, and free light chain has not been performed. The intent of this study is to better understand the components of the renal response criteria.
Patients who underwent autologous stem cell transplantation from 1995 to 2010 were eligible for this retrospective analysis if they had > 1 year of follow-up and a baseline 24 hour urine protein > 1 g/d. Those who were dialysis dependent or died before 1 year were excluded as not evaluable for renal response.
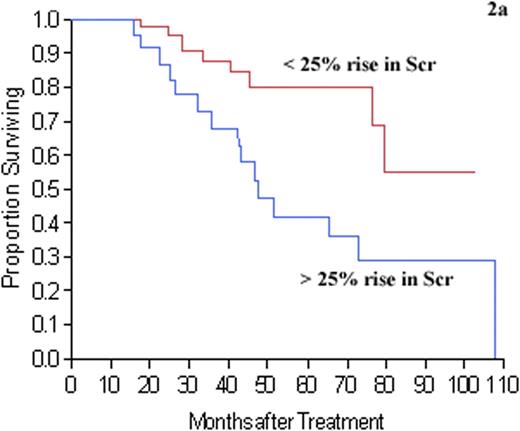
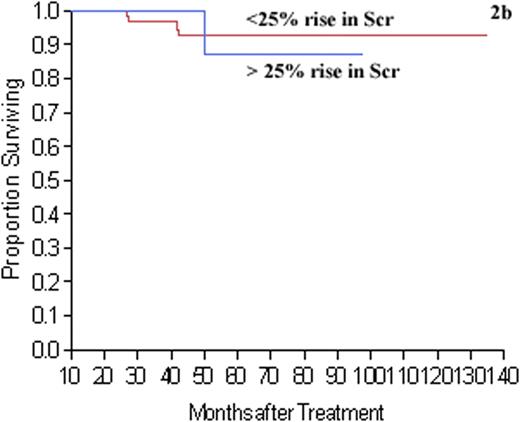
Of the 435 patients screened, 152 met criteria. On univariate analysis, >50% proteinuria reduction (p < 0.001), serum free light chain (sFLC) reduction by >50% (p = 0.002), <25% increase in serum creatinine (Scr) (p = 0.0003), and a 50% proteinuria reduction within 15 months of treatment (p = 0.04) were associated with better OS. Multivariate analysis using a proportional hazard model showed that sFLC reduction by >50% (0.006), <25% increase in serum creatinine (Scr) (p = 0.0005) and >50% proteinuria reduction (p = 0.0006) were independently associated with OS. In addition, OS was significantly better among patients achieving >85% reduction in proteinuria than those with < 85% but >50%, p = 0.03 (Figure 1). Patients with >75% reduction in sFLC were more likely to achieve >50% proteinuria reduction (p = 0.009). Most importantly, among those with > 25% increase in Scr, only those patients who had <85% proteinuria reduction had a worse OS (Figure 2a, p = 0.006). There was no difference in OS among those with >85% proteinuria reduction and a rise in Scr of > 25% (Figure 2b, p = 0.77).
Renal response is an excellent prognostic marker in patients with AL. This is the first study to show the depth of renal response correlates with OS. Patients who had the highest levels of proteinuria reduction (> 85%) had a significantly better OS than those with >50% but <85%. We also found that the negative impact of >25% decrease in renal function was only pertinent in those who did not have >85% reduction in proteinuria. These findings should help better refine the definition of renal response criteria in AL patients.
The depth of proteinuria reduction was strongly associated with the overall survival (OS) of AL patients. Patients with the highest degree of proteinuria reduction (>85%) had OS that was significantly better than patients with <85% but >50% (p = 0.02). Similarly, the OS of patients with <85% but >50% was superior to patients with <50% (p = 0.03).
The depth of proteinuria reduction was strongly associated with the overall survival (OS) of AL patients. Patients with the highest degree of proteinuria reduction (>85%) had OS that was significantly better than patients with <85% but >50% (p = 0.02). Similarly, the OS of patients with <85% but >50% was superior to patients with <50% (p = 0.03).
Decrease in renal function as signified by serum creatinine (Scr) elevation of > 25% was associated with inferior overall survival (OS) in AL patients. However, the OS was significantly affected only in patients who did not achieved >85% reduction of proteinuria (p = 0.006). In patients with > 85% reduction of proteinuria, elevation of Scr of > 25% did not affect OS (p = 0.78).
Decrease in renal function as signified by serum creatinine (Scr) elevation of > 25% was associated with inferior overall survival (OS) in AL patients. However, the OS was significantly affected only in patients who did not achieved >85% reduction of proteinuria (p = 0.006). In patients with > 85% reduction of proteinuria, elevation of Scr of > 25% did not affect OS (p = 0.78).
Leung:Binding Site: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal