Abstract
Abstract 2840
Recent studies using sensitive flow cytometry methods have reported up to 14% MBL prevalence among older adults. Although MBL has been detected in donated blood, a systematic study of MBL prevalence in blood donors is lacking. We initiated the first such study, using high sensitivity immunophenotyping and ensuring exclusion of repeat donors. Here we report results from the first ten months.
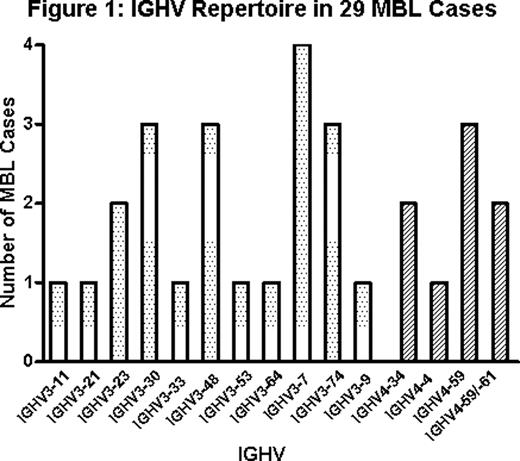
Starting in May 2010, samples from 1090 blood donors over 44 years old were collected at a regional U.S. blood center. Samples were immunophenotyped by flow cytometry with a six-color antibody cocktail (CD19, CD20, CD5, CD45 and κ/λ immunoglobulin light chains). At least 500, 000 events were collected on a FACS Canto II flow cytometer. Histograms were examined for phenotypic patterns consistent with B cell clonality. Samples were classified as MBL when at least 50 clonal B cells were detected. MBL immunophenotypes were categorized into typical chronic lymphocytic leukemia (CLL)-like, atypical CLL-like, or non-CLL-like (CD5 negative). Samples from MBL cases underwent PCR amplification, and IGHV- IGHD- IGHJ gene rearrangements were sequenced when possible.
The overall MBL prevalence (Table 1) was 7.7% (84/1090). The sex-specific prevalence was 4.2% in women and 10.2% in men. The prevalence increased with increasing age for men. In women the prevalence increased sharply from the 45–54 age group to the 55–64 age group. The prevalence in the >64 age group of women appeared to drop, but this estimate is unreliable due to the small number of observations. Multivariate log-binomial regression modeling showed that male sex and increasing age are independent risk factors for MBL: the age-adjusted prevalence ratio for sex (men/women) was 2.3 (95%CI 1.4–3.7; p=0.001), while the sex-adjusted prevalence ratio for age group 65 and older compared to the youngest age group (45–54) was 2.1 (95%CI 1.2–3.7; p=0.006).
The median absolute B-cell count was comparable in blood donors with and without MBL (167/μl vs. 160/μl). The clonal B-cell count in donors with MBL was low (median 11/μl, 10th-90th percentiles 1–122). However, the clonal count was much higher (median 333/μl, 10th-90th percentiles 90–2887) in the subset of MBL donors in whom more than 80% of the B-cells were clonal. Moreover, the clonal B-cell counts in atypical CLL-like and non-CLL-like MBL were higher (median 37/μl, n=31) than in typical CLL-like MBL (median 4/μl, n=53) (p=0.0002).
This study has so far revealed a much higher prevalence of MBL in donated blood than previously reported. The majority of MBL in this population are mutated, CLL-like, low count MBL, which has also been seen in residential population studies. These findings suggest that MBL in donated blood typically represents indolent MBL rather than clinical MBL. However, the biology of MBL is still being elucidated. Given the reported association (Castillo et al, Blood 2010) between red blood cell transfusions and non-Hodgkin lymphoma (particularly the aggregate category CLL/SLL), our findings underscore the need to ascertain long-term outcomes in recipients of blood from MBL donors. In addition, these results will be important in interpreting findings from other studies of MBL prevalence and risk factors.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal