Abstract
Abstract 2802
Therapy-related myelodysplastic syndromes and acute myelogenous leukemia (tMDS/AML) comprise a poor-risk subset of MDS/AML and are associated with a higher rate of cytogenetic abnormalities and complex karyotypes. Large scale mutation profiling efforts in de novo MDS have identified mutations that correlate with clinical features but such mutations have not been investigated in tMDS/AML.
Cryopreserved (mononuclear cell fractions) bone marrow and peripheral blood samples from tMDS/AML patients were analyzed. Lymphocytes were depleted from these fractions by either fluorescence-activated cell sorting or affinity column selection. Genomic DNA was subjected to high throughput PCR and sequenced for TP53, TET2, DNMT3a, ASXL1, IDH1, IDH2, SF3B1, EZH2, EED, SUZ12, and RBBP4. Somatic mutations were validated by comparison to lymphocyte DNA controls. Patient selection was based on sample availability for tMDS/AML patients with untreated or active, previously treated disease. Results were correlated with clinical outcomes, cytogenetic profiles, and response to therapy.
Samples from 38 patients (20 males, 18 females) with tMDS/AML were analyzed. For their primary malignancy (≥ 2 malignancies, n=3; AML, n=1; breast, n=4; colorectal, n=3; Hodgkins or composite lymphoma, n=3; gastric, n=1; melanoma, n=2; NHL, n=12; ovarian, n=1; prostate, n=3; sarcoma, n=2; thyroid, n=3), patients received chemotherapy alone (n=17), radiation alone (n=4), radioactive iodine alone (n=1), chemotherapy plus radiotherapy (n=13), radiotherapy plus radioactive iodine (n=1), chemotherapy plus radiotherapy plus radioactive iodine (n=2). Median latency time between primary malignancy treatment and MDS diagnosis date was 5.68yrs (range, 0.71–30.88). Median age at MDS diagnosis was 65yrs (range, 34–83). Not surprising was the finding that of the 35 MDS patients with complete IPSS parameter data most were IPSS Int-2 (45%) or High Risk (13%) compared to Low (11%) or Int-1 Risk (24%) disease, and in contrast to expected proportions at diagnosis for de novo MDS. WHO Classifications were: RA, n=3; RCMD, n=11; RAEB-1, n=7; RAEB-2, n=7; AML, n=3; CMML-1, n=1; MDS-U, n=3; Unknown, n=3. The median survival was 16.8mo. Median time between MDS diagnosis and sample procurement was 3.0mo (range, 0–57.2) during which 2 patients progressed to AML, 11 received a DNA methyltransferase inhibitor (DNMTI), 1 induction chemotherapy, and 2 DNMTI plus induction.
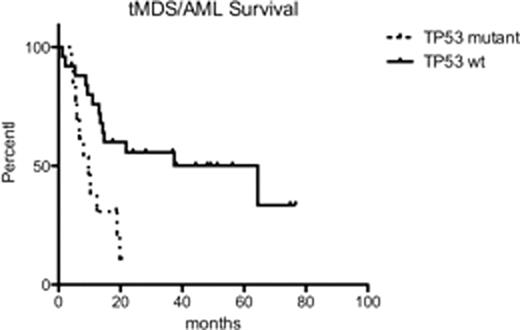
We identified somatic mutations in 15/38 (39.5%) patients. Including cytogenetic abnormalities, we identified somatic alterations in 34/38 (88%) of the patients in this cohort. TP53 mutations were most common, detected in 8/38 (21%) patients, followed by TET2 in 4/38 (10.5%), DNMT3a in 3/38 (7.9%), ASXL1 in 1/38 (2.6%), IDH1 in 1/38 (2.6%), and EZH2 in 1/38 (2.6%). No IDH2, SF3B1, EED, SUZ12, or RBBP4 mutations were detected. Only 2 patients had concurrent point mutations (one patient with TP53/TET2/DNMT3 mutations and one patient with TET2/EZH2 mutations). 7/38 (18.4%) patients had TP53 loss by FISH analysis or exhibited loss of chromosome 17/17p; 2 of these patients showed concurrent TP53 point mutations consistent with biallelic TP53 loss. 12/13 patients with TP53 abnormalities (point mutations, loss of TP53 by FISH, or loss of chromosome 17) had IPSS Poor Risk cytogenetics and 11/13 patients had abnormalities in chromosome 5 (del 5q or monosomy 5). In patients without TP53 abnormalities, 9/25 had Poor Risk cytogenetics and 5/25 had abnormalities in chromosome 5. The median survival for patients with TP53 abnormalities was 9.7mo compared to 64.4mo for patients with no TP53 abnormalities (p=0.0043). Of the 13 patients with TP53 abnormalities, 12 received treatment for tMDS/AML. 3/12 were refractory to the first line of therapy, and 7 were unable to receive an adequate course of therapy with hypomethylating agents due to toxicity or progressive disease.
TP53 point mutations are more common in tMDS/AML than in de novo MDS (7.5%, Bejar et al) while incidence of TET2 and ASXL1 mutations were lower in tMDS/AML compared to de novo MDS (20.5% and 14.4%, respectively). TP53 and TET2 point mutations were more strongly associated with exposure to prior chemotherapy, but not with exposure to radiation therapy. Taken together, these data demonstrate that TP53 mutations are common in tMDS/AML and are correlated with adverse clinical outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal