Abstract
Abstract 2625
Survival rates for eHL (most commonly defined as age over 60 years) are significantly and disproportionately inferior to those achieved in younger patients (pts). Reported 5-year event-free survival (EFS) rates for advanced-stage eHL have historically ranged from 30%–45% with 5-year overall survival (OS) rates of 40%–55%. Potential explanations for these discrepant inferior outcomes include co-morbidities precluding delivery of chemotherapy, treatment-related toxicities, and biology of disease. Data examining toxicity, survival, and prognostication for eHL in the modern era are lacking.
We report a multicenter collaboration that retrospectively investigated a large cohort of eHL pts treated over a recent 12-year period (June 1999 December 2010). We examined clinical characteristics, treatment-related toxicities, and outcomes. Furthermore, comorbidities were assessed using the Cumulative Illness Rating Scale for Geriatrics (CIRS-G) scale. Patients were also classified as “fit” vs “not fit” (i.e., loss of activities of daily living (ADLs), >3 grade 3 CIRS-G, any grade 4, and/or presence of geriatric syndrome). Univariate associations with survival were determined, while a multivariate Cox proportional hazards model was completed. Additionally, a prognostic model was constructed by classification and regression tree (CART) analysis.
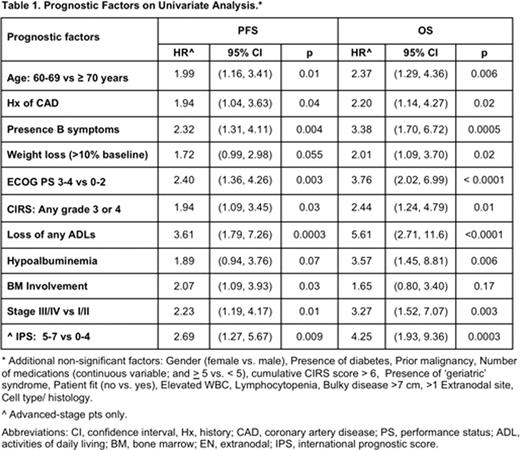
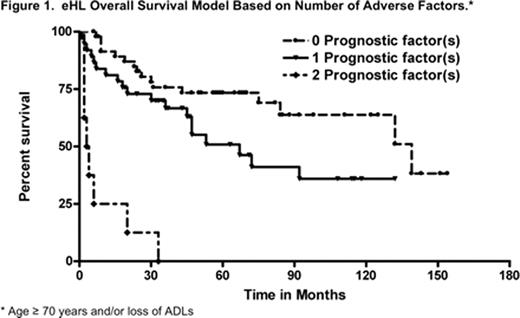
113 eligible pts were identified, while 95 had full data and were analyzed. Among these 95 pts (58M:37F), median age was 67 years (range, 60–89), with 33% of pts ages 70–79 years, while 7% were 80–89 years. 27% of pts had a prior malignancy at a median of 8.4 years (range, 1–25 years) prior to HL diagnosis, for which most had received radiation. At HL diagnosis, there were presence of B symptoms in 54%, performance status 2–4 in 27%, 21% with history of coronary artery disease, and 16% had diabetes. In terms of functional status, 61% of pts had a CIRS-G grade 3 or 4 in at least 1 category, while 46% had a cumulative score >6. Further, 17% had presence of a geriatric syndrome, 26% were classified as 'not fit', and 13% had loss of ADLs at time of HL diagnosis. 25% of pts had bone marrow involvement, while 20% had other extranodal disease (most common: bone and lung). Altogether, 64% of pts had stage III/IV disease, of which 58% had an international prognostic score (IPS) of 4–7. HL histology was nodular sclerosis in 47%, mixed cellularity 31%, NOS 16%, lymphocyte predominant 5%, and lymphocyte depleted 1%. Primary treatment consisted of: ABVD-based (n=67), MOPP-based (n=6), BCVPP (n=6), ChlVPP (n=5), radiation alone (n=4), CHOP (n=3), hospice (n=2), BEACOPP (n=1), and watchful waiting (n=1). 78% of pts received granulocyte-colony stimulating factor (G-CSF) with therapy. The overall response rate (ORR) among treated pts was 85% (73% complete remission (CR) rate). In terms of toxicity, the incidence of bleomycin lung toxicity (BLT) was 32%, which had an associated mortality rate of 25%. Notably, the incidence of BLT was 37% vs 0% among pts who received G-CSF vs not, respectively (p=0.041). With a median follow-up of 66 months (6–154) months, the 5-year EFS and OS for all eHL pts were 44% and 58%, respectively (stage I/II: 61% and 79%; and stage III/IV: 36% and 46%; p=0.009 and p=0.001, respectively). Prognostic factors that predicted survival on univariate analysis are detailed in Table 1. On multivariate regression analysis, 2 factors were associated with inferior survival: 1) age ≥ 70 years (EFS: 1.76 (95%CI 0.98–3.16), p=0.06; and OS: 2.24 (95%CI 1.16–4.33), p=0.02) and 2) Loss of ADLs (EFS: 2.47 (95%CI 0.98–6.21), p=0.055; and OS: 2.71 (95%CI 1.07–6.84), p=0.04). Furthermore, a survival model by multivariate CART analysis, based on number of these 2 adverse factors (0, 1, 2), was formed: 5-year EFS 73%, 51%, 0%, respectively (p<0.0001), and 5-year OS 93%, 68%, 11%, respectively (p<0.0001) (Figure 1).
This large, retrospective multicenter analysis of eHL found a high ORR and CR rate, but poor long-term outcomes. As shown previously, a significant percentage of eHL pts suffered BLT, which was fatal in 25% and appeared strongly related to use of growth factors. Further, several geriatric specific variables, including loss of ADL's, was highly predictive of outcome and should be prospectively incorporated into clinical trials. Finally, we developed a new prognostic model for eHL that identifies pt populations with markedly divergent outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal