Abstract
Abstract  2283
2283
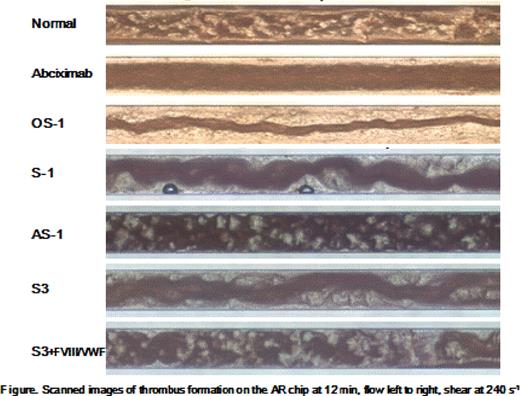
von Willebrand factor (VWF) acts as bridging molecule between platelets and vessel wall or as a career for plasma factor VIII (FVIII). Earlier reports using flow chamber had revealed that VWF acts as an “initiator” through its interactionwith glycoprotein (GP) Ib, whereas fibrinogen, via its binding to GP IIb-IIIa, acts as a “stabilizer” against high shear. VWD is categorized as partial or complete quantitative defect (type 1 or 3) or qualitative defect (type 2) of VWF based on laboratory tests, such as VWF antigen (VWF:Ag), VWF ristocetin cofactor activity (VWF:RCo), and FVIII activity (FVIII:C). However, the diagnosis of VWD remains difficult because the clinical and laboratory phenotype has wide-spectrum. An assay reflecting clinical phenotypes of VWD and effect of the treatment would be helpful for clinicians. Methods: We evaluated a thrombus formation with a new applicative microchip flow chamber instrument, total-thrombus-formation analysis system (T-TAS®). Citrated or hirudin-added blood from healthy volunteers (n=5) or 3 patients with VWD [symptomatic type 1 (S-1), asymptomatic type 1 (AS-1), and symptomatic type 3 (S-3)] were utilized. Normal blood was mixed with inhibitor for GP Ib (OS-1), GP IIb-IIIa (abciximab) and monoclonal antibody against for VWF (mAb-VWF). Patients' blood was infused with FVIII/VWF concentrates in (ex) vivo. Re-calcified citrated blood (450 μl) added corn trypsin inhibitor (30 μg/ml) was infused to AR chip of T-TAS at constant flow rate (240–600 s−1), which surface was coated by collagen and tissue factor. Hirudin-added blood (350 μl) was infused to PL chip of T-TAS at higher shear (1,000–2,000 s−1) which surface was coated by collagen. Flow pressure curve was plotted and time to 10 kPa (T10) was evaluated. Furthermore, flow images were recorded with a micro camera. AR chip promoted white thrombus formation (WTF) which reflected both platelet aggregation and fibrin generation, whilst PL chip did only platelet thrombus formation (PTF). Rotational thromboerastometry (ROTEM) were simultaneously investigated. Results: Both abciximab (0.5–2.0 μg/ml) and OS-1 (100–400 nM) inhibited WTF in AR chip dose-dependently. OS-1 (200 nM) inhibited WTF partially at 240 s−1 (T10 15.4±1.6 min, control 8.9±0.4 min), but completely at 600 s−1 (T10 >30 min, control 7.5±0.2 min). In PL chip, both agents inhibited PTF at much lower dose than those in AR chip. ROTEM parameters showed little change in both agents. Using mAb-VWF, similar results to OS-1 were obtained. These data showed that GP Ib-VWF interaction was shear-dependent, consistent with earlier reports. In in (ex) vivo assays, S-1 and AS-1 had comparable VWF levels (VWF:Ag/VWF:RCo 20%/6.4% and 5.8%/3.2%, respectively) in spite of clear difference of clinical phenotype. ROTEM parameters of S-1 were rather better than those of AS-1 likely reflecting FVIII:C (60% and 7.2%). Interestingly, however, PTF in PL chip (at 1,000 s−1) showed significant delay of T10 in S-1 (9.0 min, control 4.1±0.5 min) compared to AS-1 (5.2 min) and after in vivo infusion of FVIII/VWF concentrates, T10 in S-1 was improved (5.0 min). In S-3, ROTEM parameters declined reflecting low FVIII:C (1.2%), and prolonged T10 (>30 min) in AR chip likely reflected complete defect of VWF:Ag (<1.0%) and VWF:RCo (<1.6%). Ex vivo infusion of FVIII concentrates improved ROTEM parameters but not T-TAS parameters, whilst infusion of FVIII/VWF concentrates improved both parameters. Interestingly, scanned images with micro camera in OS-1, mAb-VWF, S-1 and S-3 was quite similar, whilst the image of AS-1 was similar to normal control. S-3 showed the normal images after infusions of FVIII/VWF concentrates (Figure). Conclusion: T-TAS has potentials for diagnosis of VWD reflecting clinical phenotypes and for monitoring the drug effects. Further, AR chip of T-TAS might have a possibility of being a potent tool for categorizing wide-range bleeding disorders “at a glance”.
Hosokawa:Fujimori Kogyo: Employment. Nogami:Bayer Award 2009: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal