Abstract
Abstract 2071
Venous thromboembolism (VTE) risk is increased in patients with malignancy, occurring in up to 20%, and is a major cause of cancer mortality. VTE prophylaxis is currently recommended for inpatients with malignancy and in those undergoing surgery (Chest 2008). Despite evidence that low molecular weight heparin (LWMH) has anti-tumor effect and improves short-term survival (Cochrane, 2011), the cost-effectiveness of anticoagulation in ambulatory cancer patients is unknown.
We constructed a Markov model to evaluate prophylactic AC in ambulatory cancer patients with no previous VTE, during 4 months of chemotherapy following diagnosis. In the model, AC was enoxaparin. Major and minor bleeding risk, VTE risk, mortality, and other clinical parameters were obtained from the Cochrane 2011 analysis and other published studies. Drug costs were based on average wholesale price. Outcomes included medical costs, effectiveness measured by mortality reduction, quality-adjusted life-years (QALY), and incremental cost-effectiveness ratio (ICER) over a 24-month time horizon.
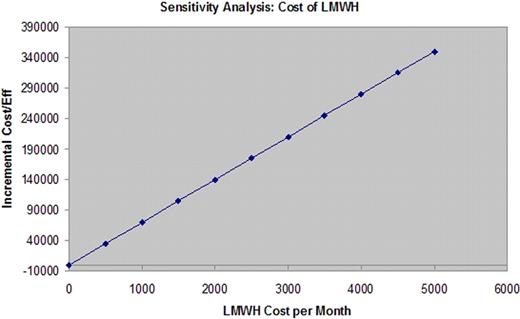
Base case results are shown in the Table. Compared with no LMWH, primary prophylaxis with LMWH in ambulatory cancer patients over a 4-month period was associated with a relative mortality risk of 0.92 over 24 months (relative risk reduction of 0.08), at a gain of 0.0484 QALY, for an ICER of $76,922/QALY gained, well within the accepted $100,000/QALY threshold. The results were not sensitive to variation in VTE relative risk (RR) with AC (base case RR 0.55), nor to AC-associated major bleeding (base case RR 1.3) or minor bleeding (base case RR 1.05) risks. Variation of the relative mortality risk with AC to ≥ 0.94, or the cost of AC (Figure) to ≥ $1,429/month (base $1,132), increased the ICER to >$100,000/QALY.
Prophylactic AC appears cost-effective in ambulatory cancer patients during the first four months of chemotherapy. Clinical trials will be needed to confirm the survival benefit of LMWH prophylaxis in ambulatory cancer patients.
| Strategy . | Cost . | Incremental Cost . | Effectiveness . | Incremental Effectiveness . | Incremental C/E Ratio (ICER) . |
|---|---|---|---|---|---|
| (1) No LMWH | $149.20 | – | 0.8215 | – | – |
| (2) LWMH | $3,874.90 | $3,725.60 | 0.8700 | 0.0484 | $76,922 |
| Strategy . | Cost . | Incremental Cost . | Effectiveness . | Incremental Effectiveness . | Incremental C/E Ratio (ICER) . |
|---|---|---|---|---|---|
| (1) No LMWH | $149.20 | – | 0.8215 | – | – |
| (2) LWMH | $3,874.90 | $3,725.60 | 0.8700 | 0.0484 | $76,922 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal