Abstract
Abstract 2018
High-dose melphalan and autologous transplantation (HDM-AT) is the most effective treatment for survival benefits in multiple myeloma (MM) patients. However, the relationship between the HDM-AT response and long-term outcome is not clear. In this study we examined the relationship.
We analyzed the clinical data of 137 patients treated with HDM-AT in three institutions between 2000 and 2011. The international Myeloma Working Group Uniform Response Criteria was used to evaluate.
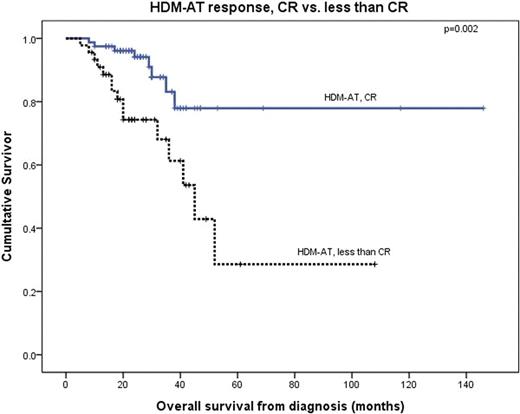
Out of 137 patients, clinical data of 126 patients were evaluable for treatment response according to the medical records. Their median age was 55 years (range, 36–65 years) and 69 (55%) patients were male. Among the patients who had received induction treatment (IT), 79%(100/126) of the patients were treated with bortezomib-containing regimens. After IT, the response rates were 29% CR, 18% VGPR, 37% PR, 15% SD, and 1% PD. After HDM-AT, response rates were 64% CR, 15% VGPR, 15% PR, 4% SD, and 2% PD. Median follow-up duration was 25 months (range, 5–146 months). 5-year overall survival (OS) and progression-free survival (PFS) were 54% and 43 %, respectively. Multivariate analysis regarding OS showed that CR after HDM-AT compared to ≤CR is an important prognostic factor (5-year OS rate of CR vs ≤CR, 78% vs 29%, respectively, p=0.002). However, CR after HDM-AT is not prognostic factor for PFS.
79 (79/126, 64%) patients showed the CR after HDM-AT. Among the 79 patients, 44 patients did not achieve CR after IT however, turned into CR after HDM-AT; 35 patients already achieved CR after IT. However, there were no significant differences between the two groups of patients (5-year PFS, 44% vs. 45%, P=0.245 and 5-year OS 77% vs. 79%, P=0.690 respectively).
Achievement CR after HDM-AT is the only important prognostic factor to obtain the survival benefit regardless of response after IT in MM patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal