Abstract
Abstract 2001
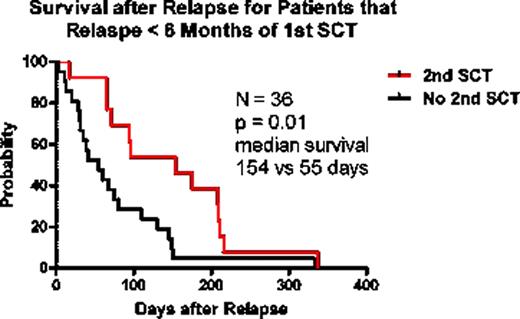
Patients with leukemia relapsing after SCT have a dismal prognosis. Treatments ranging in intensity from palliation to second SCT are offered to such patients but the overall survival remains in the region of 3–4 months. Second SCT is typically restricted to selected patients deemed more likely to survive and experience further leukemia control. However, since a second SCT is associated with an increase risk of transplant related morbidity and mortality, it is important to determine whether this option has a survival benefit. We studied 60 consecutive relapsed patients who had received a myeloablative matched-sibling T-cell depleted SCT for a variety of hematological malignancies including AML, ALL, CML blastic phase, and MDS. Median patient age at time of first SCT was 36 years (range, 10 – 68), median T cell dose varied between 1–5 x104/kg. Thirty-five patients relapsed early (< 6 months post SCT) with a median survival after relapse of 170 days (range 45 – 402), and 25 patients relapsed late (> 6 months post SCT) with a median survival after relapse of 1005 days (range, 240 – 4459). Salvage therapies included tyrosine kinase inhibitors (for CML), intrathecal chemotherapy (for CNS leukemia), and systemic chemotherapy combinations predominantly involving fludarabine and cytarabine. Twenty-four patients (13 early relapse, and 11 >6 months), with a good performance score and showing some preliminary response to non-transplant therapy, received a 2nd SCT from their original donor. Our rationale for selecting these patients for a T replete 2nd SCT was based on the potential enhancement of graft-versus leukemia effects following the failed T-cell depleted SCT. Sixteen received myeloablative conditioning with either Busulphan or Melphalan, and 8 patients received a nonmyeloablative regimen specific to their disease. Of the 36 patients not transplanted, 14 received a donor lymphocyte infusion, and 22 received palliative chemotherapy or hospice care only. Compared with non-transplant treatment patients, only those relapsing early after their first SCT experienced a significant but small survival benefit from 2nd SCT, with most patients dying from relapsed disease (median 55 vs 154 days, untransplanted vs transplanted; HR = 0.4, p = 0.01). In untransplanted patients survival was not different between any treatment option. Although patients selected for 2nd SCT represented a more favorable group, it was disappointing that intensive treatment only resulted in a 3 month prolongation of median survival. These results do not indicate an important benefit for second transplant in any patient relapsing with leukemia after SCT.
Disclosures:
No relevant conflicts of interest to declare.
Author notes
*
Asterisk with author names denotes non-ASH members.
© 2011 by The American Society of Hematology
2011

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal