Abstract
Abstract 1939
RIC SCT relies heavily on graft-versus-tumor alloreactivity, and relapse remains a major barrier to a favorable outcome. Early prediction of relapse would allow early intervention such as donor lymphocyte infusions (DLI), but factors that predict relapse and methods for detection of minimal residual disease are often disease specific and not standardized. The level of donor-recipient chimerism has been associated with both graft rejection and relapse, but the optimal timing, desired level, and predictive value of chimerism testing in RIC SCT are unclear. Furthermore, the clinical utility of whole blood (WB) vs T-cell chimerism is not well defined, particularly after RIC SCT.
We aimed to assess the predictive value of early WB and T-cell chimerism on the incidence of relapse in SCT pts receiving a uniform RIC regimen for hematologic malignancies. Between August 2006 and May 2011, 120 consecutive patients (pts) underwent allogeneic SCT following conditioning with fludarabine 120mg/m2 and busulfan i.v. 6.4 mg/kg. Pts were not treated with pre-emptive DLI, but could receive DLI for relapse. Hematopoietic chimerism was determined by DNA genotyping of short tandem repeats. Chimerism was determined on WB and then on enriched T-cells, obtained by selection using CD3-labeled magnetic beads. We conducted a cumulative incidence analysis of relapse, using day 30 as a landmark to determine the predictive properties of chimerism studies obtained at that time.
The 1-yr cumulative incidence of relapse in this cohort was 48.3 ± 4.7%, and the median time to relapse was 102 days (range 16–566 days), highlighting the importance of early monitoring. 68 pts were in remission and had evaluable chimerism data on day 30; importantly, the 1-year incidence of relapse was not different between pts who did and did not have day 30 chimerism measured (50.2 ± 6.5% vs. 42.9 ± 7.2%, P=0.45). Median follow up was 238 days (range 75–1420). Median age was 61 (range 21–76) and 56% were male. Underlying diseases were AML (24), MDS (13), NHL (10), myelofibrosis (6), CTCL (4), Hodgkin (3), myeloma (3), CLL (2), aplastic anemia (2), CML (1). Pts received a peripheral blood stem cell graft (67) or bone marrow (1), harvested from a matched related (30) or unrelated (38) donor. A single antigen mismatch was present in 6 cases. GVHD prophylaxis was tacrolimus (55) or cyclosporine (13) based.
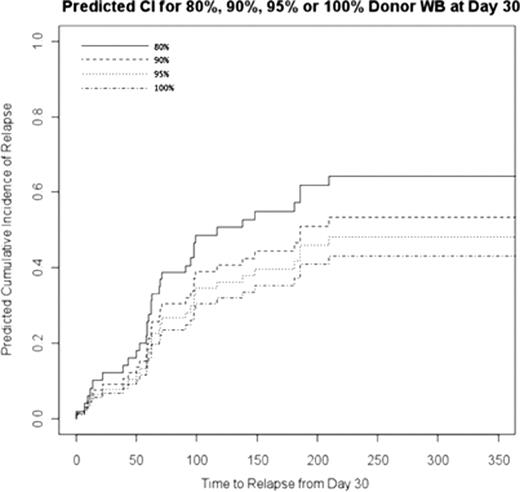
Median WB donor chimerism at day 30 was 96% (range 31–100%). A cumulative incidence analysis of relapse from day 30 revealed that day 30 WB chimerism had a significant association with relapse (HR 0.97, 95% CI [0.95–0.99], P=0.0011), reflecting a 3% decrease in risk of relapse for each 1% increase in chimerism. Risk of relapse according to different day 30 chimerism levels is displayed in figure 1. Using a day 30 chimerism cutoff of 95%, we found a significant association with incidence of relapse (HR 0.29, 95% CI [0.15–0.57), P=0.0003). Pts who were alive without relapse at the end of follow-up had a significantly higher chance of >= 95% day 30 WB chimerism compared to pts who relapsed (88.9% vs. 45.5%, P=0.002). In 38 pts with myeloid diseases, there was a significant association between day 30 WB chimerism and risk of relapse (HR 0.97, 95% CI [0.96–0.99], P=0.00065), while in 22 pts with lymphoid diseases, an association did not reach statistical significance (HR 0.93, 95% CI [0.84–1.00], P=0.09).
Median T-cell chimerism was 70% in the 49 evaluable pts with these measurements (range 26–99%). T-cell chimerism on day 30 did not predict relapse (HR 1.0, 95% CI [0.98–1.02], P=0.95).
We analyzed potential associations between day 30 WB chimerism and various transplant and patient characteristics. A higher chimerism level was significantly associated with lower day 0 lymphocyte count (P=0.004) and lower preconditioning lymphocyte count (P=0.01), but was not associated with recipient or donor age, cell doses, busulfan levels, disease type and donor type. The day 0 lymphocyte count was also a strong predictor of relapse (HR 6.87, 95% CI [6.56–7.04], P=0.00035).
Whole blood and not T-cell chimerism at day 30 is predictive of relapse after RIC SCT. WB chimerism is strongly associated with lower lymphocyte counts before and after the conditioning regimen. These data highlight the importance of adequate lymphodepletion and can be useful in designing future trials testing pre-emptive interventions to prevent relapse after RIC SCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal