Abstract
Abstract 1726
Treatment of CMML remains a clinical challenge, with no drug demonstrating clear clinical benefit. AZA yielded a survival benefit in higher risk MDS in a study that included few patients with CMML (AZA 001 trial, Lancet Oncol, 2009). Several small series of CMML treated by Decitabine (Wijermans, Leuk Res. 2008, Aribi A, Cancer. 2007 and Kantarjian H, Blood. 2007) and AZA (Scott, Br J Haematol. 2010) have been reported, but numbers were small with heterogeneous risk factors.
A cohort of CMML pts (according to WHO classification) treated with AZA in 3 programs (French AZA compassionate program, Cleveland Clinic Foundation and H. Lee Moffitt Cancer Center) were reviewed. All pts received AZA for at least one cycle (75 mg/m2/d during 7 days every 28 d). Response was evaluated according to IWG 2006 criteria in patients with WBC <13G/L, but also took into account “proliferative” features of CMML (including palpable splenomegaly [SM] and white blood cell count [WBC] in patients with WBC > 13G/l), in agreement with our previous experience (Wattel, Blood 1996; Braun, Blood 2011 online).
Between 2004 and 2009, 79 CMML pts received AZA. The median age was 70 y (range 33–85), M/F: 50/29. Median interval from diagnosis to treatment was <6 months in 30 pts, 6–12 months in 10 pts and > 12 months in 34 pts. At onset of AZA, median WBC, Hb level and platelet count were 11.4 G/l (range 7–122), 10 g/dl (range 6.3–15.2) and 59 G/l (range 9–1214), respectively. According to the WHO classification, 53% were CMML1 and 47% CMML2. Forty six percent of pts had WBC > 13 G/l and 32% had palpable SM (44% pts had neither of those features, 32% pts had one and 23% had both). Among pts with WBC<13G/l, IPSS was low or int 1 in 24% pts and high or int 2 in 30%. Prior to AZA, 48% pts received previous therapy, including growth factors in 13%, hydroxyurea in 18% and intensive chemotherapy in 17% patients. Karyotype was normal (57%), with chromosome 5/7 abn (14%), and with other cytogenetic changes (29%). The median number of cycles of AZA administered was 6 (range 1–40).
Thirty-four pts (43%) responded including CR (16%), PR (1.5%), marrow CR (8%), hematological improvement (HI) (18%). Among 60 pts who received more than 4 cycles, 33 (55%) responded, including 13 (22%) who achieved CR. Patients who achieved response were significantly older (median 71 vs 66 years in non responders, p=0.0170).WBC count (p=0.4241), WBC >13 G/L (p=0.483), Hb level (p= 0.4529), platelet count (p= 0.1658), marrow blast % (p=0.4278), palpable SM (p= 0.319), cytogenetics (p=0.947), disease duration (p= 0.808), prior therapy (p= 0.277) and prior therapy excluding GF (p= 0.147) had no impact on response. Twenty-six patients progressed to AML after a median of 630 d (range 85–1165 d), including 12/34 of the responders (6 CR, 1 PR and 5 HI).
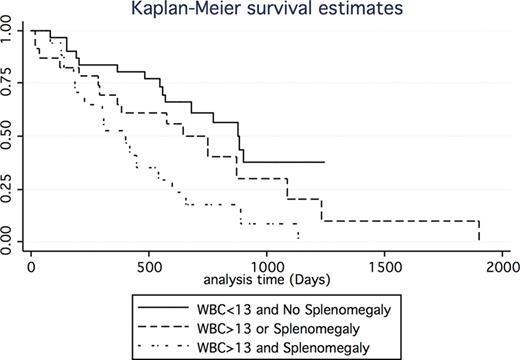
The median overall survival (OS) from initiation of AZA (OS) was 654 d. In univariate analysis, prior therapy when ESA were excluded (p=0.0488), palpable SM (median 420 d vs 870 d, p= 0.0230), WBC>13 G/l (420 vs 775, p= 0.0412), presence of palpable SM and/ or WBC>13G/l (none: median 876d vs either: 750d vs both: 401d, p= 0.0054) (figure 1) IPSS in pts with WBC<13 G/l (1085d for low /int1 vs 682 for high/ int2, p= 0.0046), marrow blast >10 % (383d vs 682d, p=0.028) significantly influenced OS while Karyotype (p=0.4217), sex (p= 0.5174) and Hb level had no influence on OS. By multivariate analysis, only marrow blasts>10 % (HR=2.19 (1.13–4.2), p=0.02) and presence of proliferative features (WBC>13G/L and/or palpable SM) (HR= 2.08 (.94 −4.6),p= 0.06) had prognostic value for OS. Finally, using a landmark analysis performed at 3 mo, Patients who achieved a response had a significantly better OS compared to patients who failed to respond (median 889 d vs 569 d, p= 0.047).
In this population of CMML patients with generally poor prognostic features, the response rates (ORR 43%) and overall survival (21 mo) with AZA treatment was similar to that previously reported in higher risk MDS. No significant predictive factors for response to AZA were identified, but marrow blast % and proliferative features (including increased WBC count and/or splenomegaly) were adverse prognostic factors for survival.
Sekeres:Celgene: Membership on an entity's Board of Directors or advisory committees. Maciejewski:Celgene: Membership on an entity's Board of Directors or advisory committees. List:Celegene: Consultancy. Fenaux:Celgene: Membership on an entity's Board of Directors or advisory committees. Komrokji:Celgene: Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal