Abstract
Abstract 1692
There has been a remarkable improvement in the management of chronic myeloid leukemia (CML) after imatinib mesylate (IM) became available in the market, but there is still a group of patients who are resistant to imatinib. Although point mutations in the BCR-ABL kinase domain is the most common mechanism for resistance in patients with CML receiving tyrosine kinase inhibitor (TKI) therapy, there are several mechanisms that can play a role in the resistance to TKIs. Multi drug resistance gene (MDR1) [ABCB1 (ATP-binding cassette, sub-family B (MDR/TAP), member 1) ] product is an ATP-driven efflux pump contributing to the pharmacokinetics of drugs that are P-glycoprotein (P-gp) substrates and to the multidrug resistance of cancer cells. More than 50 single nucleotide polymorphisms (SNPs) have been identified concerning the MDR1 gene, and SNP polymorphisms may affect the expression and function of the P-gp. The SNPs T1236C, G2677T/A, and C3435T are the most common variants in the coding region of ABCB1. Imatinib is a substrate of P-gp-mediated efflux, and P-gp mediated drug efflux can play a role in IM resistance. So identifying these SNPs may allow to predict the drug disposition and responses to IM in CML patients. The aim of the study was to identify the C3435T SNP variants, and the associations between MDR1 C3435T polymorphism and IM efficacy in our CML patients.
Between December 2010 and March 2011, 110 chronic phase (CP) CML patients who consecutively visited our outpatient clinic were enrolled in this study. Hematologic, cytogenetic and molecular response patterns to IM as well as the association between MDR1 C3435T polymorphism and responses to imatinib were evaluated in our patient cohort. MDR1 C3435T polymorphisms were detected by real-time polymerase chain reaction (RT-PCR). We could assess complete cytogenetic response (CCyR) and major molecular response (MMR) in one hundred and six patients (96%) among these 110 patients. The differences in genotype frequencies in all patients taking imatinib treatment was determined by using the chi-square test. All tests were two-sided, and p <0.05 was considered as statistical significant. This study was approved by the local research ethics committee, and written informed consent was obtained from the patients.
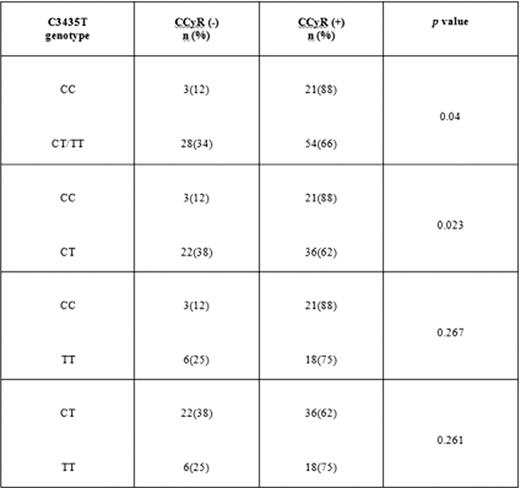
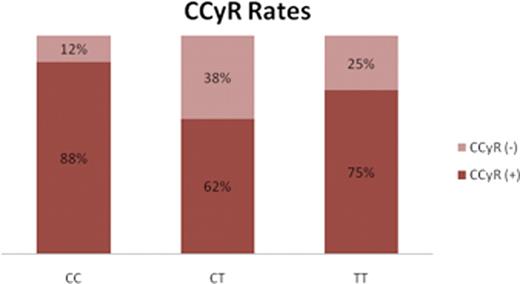
59 patients were male (54%), and fifty-one were female (46%). Median age was 50.5 years (range, 19–84 years). 37.6% of the patients were low, 45% were intermediate, and 17.4% were high risk according to Sokal risk score. The CCyR rate was 71%, and MMR rate was 60%. The frequencies of MDR1 3435 CC, CT, and TT genotypes were 22.5%, 55%, and 22.5%, respectively. No statistically significant difference was observed between the frequencies of the genotypes according to gender. The CCyR rates in patients with CC, CT, and TT genotypes were 88%, 62%, and 75%, respectively (Figure 1). The patients with CC genotype had significantly higher CCyR rates when compared to patients having CT/TT and CT genotypes (p =0.04 and p =0.023, respectively) (Table 1). The patients with CC, CT, and TT genotypes did not differ significantly between each other regarding the MMR rates. There were no significant difference between the C3435T genotypes and second generation TKI usage regarding both CCyR and MMR.
The CCyR rates in different MDR1 C3435T genotypes (CCyR=complete cytogenetic response).
The CCyR rates in different MDR1 C3435T genotypes (CCyR=complete cytogenetic response).
MDR1 polymorphisms in patients with CCyR (+) or CCyR (−) under imatinib treatment (CCyR= complete cytogenetic response).
Before starting IM therapy, the individual patientÕs MDR1 gene polymorphism pattern can be important in determining the treatment strategy in patients with CML. Among our patient cohort, the patients with CC genotype had significantly higher CCyR rates than patients with CT/TT and CT genotypes. Up to now, there are a few studies in CML patients with different results regarding MDR1 gene polymorphisms, and since racial differences can be seen in the frequencies of MDR1 gene polymorphisms, further studies in larger series are needed to define the genetic polymorphisms with therapeutic relevance in patients on imatinib.
This study was supported by Istanbul University Research Fund.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal