Abstract
Abstract 1612
in follicular lymphoma (FL) patients with high tumor burden (as defined by GELF criteria), R-CHOP is the standard upfront immunochemotherapy. Results from the PRIMA study suggest that a positive PET after induction therapy predicts for earlier relapses, even despite maintenance with rituximab (RTX) for two years [Trotman J, 2011]. For patients under 65y, who relapse after R-CHOP+/−RTX maintenance with high tumor burden, R-chemo+autografting is a recommended option. In a retrospective cohort of 43 relapsed FL pts in two French University Hospitals, we explored the role of such a strategy on outcome - in the era of new RTX based modalities - and also evaluated the impact of PET results before autografting.
PATIENTS AND METHODS: Patients with relapsed FL after R-CHOP, with at least 1 GELF criteria at relapse (high tumor burden), and who received R-chemo before autografting were eligible. IWC+PETresponse criteria (Cheson 2007) were used, after R-CHOP frontline, and after salvage (before autografting). Patients with Richter transformation at relapse were excluded from this study. OS was calculated from date of salvage to date of death or last follow-up; progression-free survival (PFS) and time to next treatment (TTNT) were calculated from completion of salvage to date of FL relapse or next chemotherapy, respectively.
43 pts (60% males) younger than 65y were identified: they received either FCR-based (2 cycles of FCR, 1 cycle of R-DHAP then stem cell harvest, 2 last cycles of FCR, n=25) or R-DHAP-based (4 cycles of R-DHAP or DHAOx (oxaliplatin replacing cisplatin), and stem cell harvest, n=18).
median age was 54 (range 28–62), with median GELF score of 1 (1–4). Thirty % had progression within 6 mo of R-CHOP (refractory);median PFS was 12mo (range 1–40mo) andmedian TTNT was 15mo. RTX maintenance in 12/43 pts did not significantly increased PFS (15 vs 9 mo, p=0.1). FLIPI1 was low in 39%, Int 36%, high 25% of pts, and FLIPI2 was low in 22%, Int 62.5%, high 15.5% of pts. 1/43 pt had CD20- relapse (who received RTX maintenance), and received FC without RTX.
response to FCR/R-DHAP included CR+CRu 68/72%, PR 24/28% respectively, PET evaluation was found negative in 23.5/36% respectively (p=ns). Median stem cell harvest (median 2 leukaphereses) was 4.37 vs 7.8.106 CD34+/kg in FCR vs R-DHAP pts (Mann-Whitney p=0.09), without failure (only one patient required plerixafor). Four patients did not receive the planned autologous transplant (2 failures after FCR (including one Richter transformation), 1 hepatitis before conditioning regimen, 1 withdrawal of consent). Conditioning regimen for the remaining 39 pts was BEAM in 16 (4 FCR+12 R-DHAP), Zevalin-BEAM in 23 pts (9 FCR+14 R-DHAP), including 9 pts who further received RTX maintenance post-autografting.
At a median follow up of living pts of 18mo, 9 pts had relapsed, of which 8 needed additional therapy. At time of analysis (June 2011), 37 pts were alive. Causes for death included 1 pancytopenia and infection, 1 Richter syndrome, 1second cancer, 2 complications of allografting (received later on). Late complications were common: pancytopenia or prolonged grade III-IV neutropenia (>3mo) after procedure occurred in 5/43 pts (3 FCR, 2 R-DHAP, without evidence of MDS/AML in these cases), Richter syndrome occurred in 2 patients (1 death), second cancer in 3 pts (1 Hodgkin, 1 womb sarcoma, 1 lung cancer).
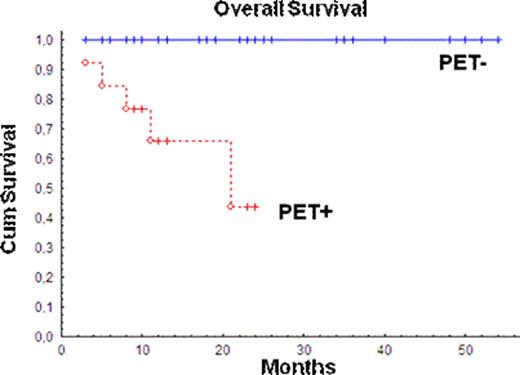
On an intend-to-treat basis, 41 pts are evaluable. For FCR/R-DHAP pts, 2y PFS was 68/68%, 2y TTNT 80/70%, and 2y OS 73/100%, respectively (logrank p=ns). Two years TTNT tended to be higher in pts receiving Z-BEAM (55 vs 83%), or with PET negativity before autografting (70 vs 85%), both without reaching significance (logrank p=0.1). PET negativity before autografting was the only variable statistically associated with superior OS in our series (logrank p=0.0003).
Our data suggest that PET negativity before consolidative autografting is an achievable and desirable goal in FL salvaged after R-CHOP.
Ysebaert:Roche: Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal