Abstract
Abstract 1601
Primary Mediastinal B-cell Lymphoma (PMBCL) is an uncommon variant of Diffuse Large B-cell Lymphoma (DLBCL). Given the rarity of this disease, data guiding management is extrapolated from DLBCL trials, or from small retrospective analyses limited to PMBCL. Prospective evaluation of R-CHOP in the MiNT trial showed excellent results in PMBCL, but this trial was limited to young low risk patients. We present the largest retrospective series to date of R-CHOP for PMBCL in all risk groups.
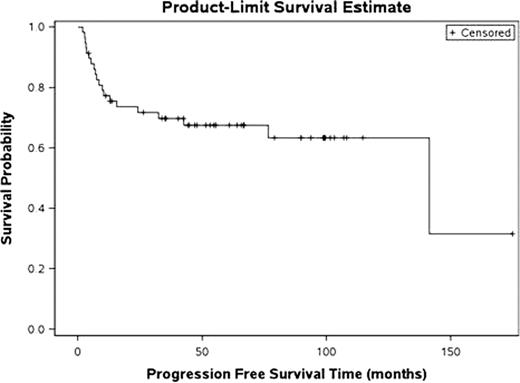
We identified cases of PMBCL at our institution using a comprehensive clinicopathologic database derived from tumor registry data. Natural language processing software was used to search pathology reports for terms of “mediastinal lymphoma,” “mediastinal large cell lymphoma,” “mediastinal large B-cell lymphoma,” as well as “lymphoma” in mediastinal biopsy specimens. Cases were included if they met clinicopathologic criteria for PMBCL, defined as a large B-cell lymphoma with typical features for PMBCL presenting with a dominant anterior mediastinal mass. All patients had to have been treated with R-CHOP. Progression-free survival (PFS) and overall survival (OS) are calculated by the Kaplan-Meier method and univariate analysis is performed to assess predictors of outcome.
Fifty-eight cases from 2000–2011 met inclusion criteria and are included in the analysis. The median age was 38 years (range 20–82) and 60% were male. Forty-four patients (76%) presented at limited Ann Arbor stage and 12 patients (21%) at advanced stage; presenting stage could not be discerned in 2 patients. Fifty-five percent of patients presented with mediastinal bulk ≥10cm in size; median size was 11cm (range 5–17cm). LDH was elevated at diagnosis in 60% of patients, normal in 21%, and unknown in 19%. By revised IPI score, 19% were low-risk (0 risk factors), 60% were intermediate risk (1–2 risk factors) and 12% were high-risk (≥3 risk factors). R-CHOP was given for a median of 6 cycles (range 1–8); 51 of 58 patients received 6 or 8 cycles. Among patients who achieved initial remission, 78% underwent consolidative radiotherapy and the remainder were observed after chemotherapy alone.
The overall response rate was 81% (90%CI [71%–89%]) with 72% complete responses and 9% partial responses. Ten patients (17%) had primary refractory disease defined as progression on treatment or within 3 months of completion of therapy. Among 46 patients who achieved a response, 5 (11%) subsequently relapsed. Two patients, both elderly, died during treatment. Among the 10 patients with primary refractory disease, 6 have died from progressive lymphoma, 2 patients are alive with active disease undergoing salvage therapy, 1 is alive and free of disease greater than 8 years from diagnosis, and 1 was lost to follow-up. Among 5 patients with relapsed disease, 2 are alive without disease at last follow-up, while 3 have died of progressive lymphoma. Median follow-up for the entire series is 58 months. Five-year PFS is 68% (95% CI, 55% to 80%) and 5-year OS is 76% (95% CI, 65% to 88%). On univariate analysis, advanced Ann Arbor stage and high R-IPI score were associated with inferior PFS and OS. (p=0.006 and p<0.001, respectively for PFS, p=0.005 and p<0.001 for OS, log-rank test).
PMBCL treated with R-CHOP carries an overall favorable prognosis, though primary refractory disease occurs in a significant number of patients, and is rarely curable with second line therapy. Advanced stage disease and high R-IPI scores are associated with inferior outcome. Novel treatment approaches warrant evaluation in high-risk patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal