Abstract
Abstract 1248
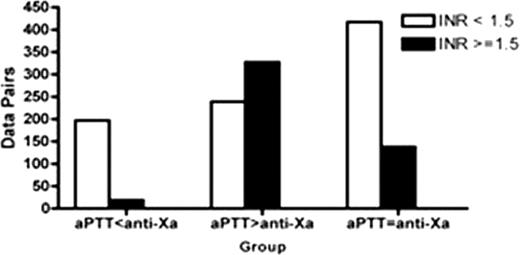
Historically, unfractionated heparin (UFH) has been monitored using the aPTT, a global measurement of the ability of the heparin-antithrombin complex to inactivate the relevant clotting factors. However, the aPTT response to heparin depends on patient variables and reagent and instrument factors. Anti-Xa activity is routinely used to calibrate aPTT for heparin therapy nomograms, and some institutions use anti-Xa activity directly in heparin dosing nomograms. In general, there is a lack of data correlating these methods of measuring heparin effect in patients and outcome data validating any particular approach. We sought to determine the concordance of aPTT and anti-Xa measurements and its impact on patient outcomes in adult hospitalized patients treated with UFH. METHODS: All simultaneously drawn aPTT and anti-Xa values from patients 18 years and older receiving UFH while hospitalized at Stanford between February 2009 and August 2009 were extracted from Stanford's patient database. We created an aPTT/anti-Xa reference curve using normal pooled plasma with heparin added at increasing concentrations from 0.05 u/mL to 1.0 u/mL, with simultaneous measurement of aPTT and anti-Xa activity. We designed a polynomial fit correlating aPTT and anti-Xa activity with a 99% confidence limit. We then grouped paired aPTT/anti-Xa values into one of three groups according to whether the paired values fell within or outside of the correlation area: 1) aPTT<anti-Xa: discordant pairs, with low aPTT to anti-Xa value, 2) aPTT> anti-Xa: discordant pairs, with high aPTT to anti-Xa value, and 3) aPTT= anti-Xa: concordant pairs, with aPTT and anti-Xa values within the correlation area. In addition, each aPTT/anti-Xa data pair which had an INR from the same date was categorized as associated with either a low (< 1.5) or high (>= 1.5) INR. Because individual patients could have data pairs that fell into multiple groups, we further narrowed the aPTT > anti-Xa and aPTT= anti-Xa groups into patient subgroups to assess outcomes, wherein each patient had data pairs only in one group. RESULTS: A total of 2321 paired values from 539 patients were studied. Data pairs were frequently discordant: 413 (18%) data pairs were in the aPTT < anti-Xa group, 971 (42%) were in the aPTT > anti-Xa group, and 937 (40%) were in the aPTT=anti-Xa group.1337 of 2321 (58%) aPTT/anti-Xa data pairs had an INR value from the same date. The aPTT>anti-Xa group had the highest proportion of data pairs associated with an INR >= 1.5 (68%, see Figure, p< 0.0001 for comparison between the three groups). Patient clinical outcomes were compared between the aPTT > anti-Xa and aPTT=anti-Xa patient subgroups. The 30-day mortality was 19 of 87 (21%) in the aPTT > anti-Xa patient group, higher than in the aPTT=anti-Xa group (6 out of 112, 5%) (p < 0.001). As warfarin use is known to increase the sensitivity of the aPTT to heparin, we compared those patients on concomitant warfarin and heparin to those on heparin alone. Patients with consistent aPTT> anti-Xa on heparin alone had the highest 30-day mortality (16 of 39, 41%), compared to a 30-day mortality of 6% (3 of 48) for aPTT > anti-Xa patients who were on both heparin and warfarin (p < 0.001). The 30-day mortality was not significantly different between those in the aPTT=anti-Xa group on heparin alone (5 of 89, 6%) compared to those on heparin and warfarin (1 of 23, 4%, p>0.05), nor was the 30-day mortality significantly different between those in the aPTT>anti-Xa on heparin and warfarin (3 of 48, 6%) compared to those in the aPTT=anti-Xa on heparin and warfarin (1 of 23, 4%, p>0.05). DISCUSSION: Simultaneously measured aPTT and anti-Xa values in a large cohort of hospitalized adult patients treated with UFH were discordant the majority of the time. The most common discordant pattern was a high aPTT to anti-Xa value. This group was associated with an INR >= 1.5 68% of the time, indicating that a baseline prolongation of the PT is associated with an increased sensitivity of the aPTT to UFH. Increased sensitivity to heparin as demonstrated by an aPTT > anti-Xa in the absence of warfarin appeared to be an indicator of poor health with significantly higher 30-day mortality from underlying disease conditions. Further study is needed to determine whether the aPTT or anti-Xa should preferentially be used in heparin dosing nomograms when the values are discrepant.
Number of data pairs in each group with a same-day INR with high and low INR values
Number of data pairs in each group with a same-day INR with high and low INR values
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal