Abstract
For patients with SCD, blood transfusion (tf) is the mainstay of treatment to prevent and alleviate SCD complications. Though the majority of patients in pediatric care often receive optimal preventive care, discrepancies are seen in care management of patients transitioning from pediatric to adult care as well as in adult patients. The study objectives were to evaluate blood transfusions patterns and incidence of SCD complications in pediatric and adult patients with a focus on those transitioning from pediatric to adult care.
State Medicaid data from the FL (1998–2009), NJ (1996–2009), MO (1997–2010), IA (1998–2010), and KS (2001–2009) were used for this study. Patients with ≥2 SCD diagnoses (ICD-9 282.6x) and ≥1 tf following the 2nd SCD diagnosis were included in the analysis. Patients were followed for as long as they were enrolled in Medicaid. Quarterly rates of tf events, SCD complications, and prescriptions of hydroxyurea were calculated. Each tf event was defined as a unique day when at least one procedure code for packed RBCs, whole blood, or exchange tf was recorded. SCD complications included pain, infection, stroke, cardiomyopathy, renal disease, and Moyamoya disease. A logistic regression was used to assess associations between tf and transition age (<18 vs ≥18 yrs), population density of living area (urban, suburban, rural), state of residence, and SCD complications. An interaction term of transition age and SCD complications was also included to isolate the impact of SCD complications on tf between the pediatric and adult periods. Other covariates included prescription of hydroxyurea, tf during the previous quarter, other relevant medications (e.g.: pain medication, diuretics, anticoagulants), comorbidities (e.g.: hypertension, myocardial infarction, liver disease), and, serving as proxies for overall health status, the frequency of hospitalizations, emergency, and outpatient visits during the previous quarter.
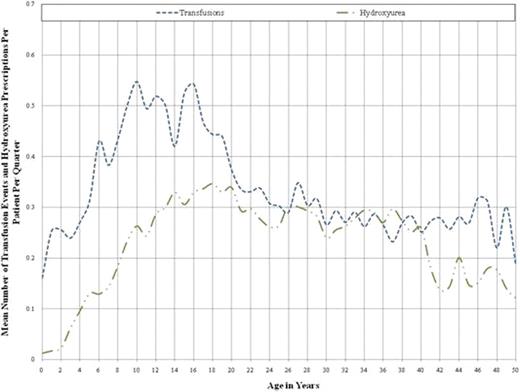
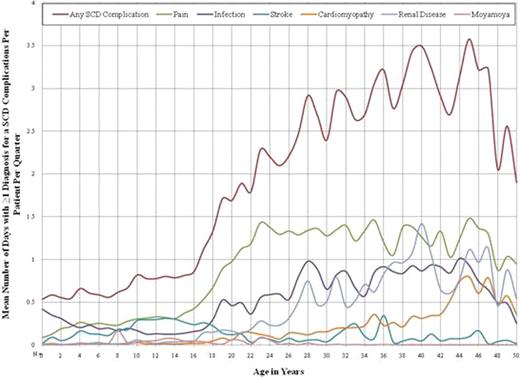
A total of 3,208 patients were included (FL: 1,550, NJ: 992, MO: 489, KS: 121, IA: 56) in the study. Each patient was observed for an average (SD) of 6.0 (3.1) years. About 73% of patients lived in an urban area, 23% lived in suburban area, and 4% lived in a rural area. The rate of tf had a distinct bimodal pattern over ages. The rate of blood tf increased from 0.25 tf/pt/quarter at 1 year of age to a maximum of 0.54 tf/pt/quarter at 16 years old (Figure 1). After age 16, the tf rate decreased sharply to 0.29 tf/pt/quarter at age 26, and remained relatively stable thereafter. In contrast, the frequency of diagnoses for SCD complications increased markedly after age 16, reaching 2.92 diagnoses/pt/quarter at 28 years old and 3.50 diagnoses/pt/quarter at 40 years old (Figure 2). Pain was the most common complication, followed by infection, and renal disease. The frequency of diagnoses for cardiomyopathy slowly increased between 18 and 42 years old from 0.05 to 0.36 diagnoses/pt/quarter and then more than doubled to reach 0.80 diagnoses/pt/quarter at age 45 (Figure 2). Hydroxyurea use increased steadily up until age 18 and declined thereafter (Figure 1). Prescriptions for pain medications rose in a linear fashion from age 15 to 35 years from an average of 0.61 prescription/pt/quarter to 3.05 prescriptions/pt/quarter, and stayed high until the end of follow up. Results from the logistic regression showed that patients were less likely to receive blood tf post transition age (odds ratio [OR], ≥18 years old: 0.85, p=.014) and when receiving hydroxyurea (OR: 0.82, p<.001). In contrast, patients were more likely to receive tf if they lived in urban or suburban areas compared to rural areas (OR, urban: 3.65; suburban: 3.40; p<.001 for both) and experienced SCD complications (OR: 2.66, p<.001). The positive association between SCD complication and tf was stronger post transition age (OR, interaction between SCD complication and older age: 1.39, p<.001).
Patients transitioning to adult care are transfused less frequently than pediatric patients and suffer from more frequent SCD related complications. These findings highlight the changes in treatment patterns corresponding to transition to adult care. While age related increases in SCD complications may be anticipated, the dramatic increase in complications along with the decline in tf frequency are likely to be due at least in part to inadequate transition to adult providers.
Blinder:Novartis: Honoraria. Vekeman:Analysis Group: Analysis group received research grant from Novartis pharmaceuticals, Employment. Trahey:Analysis Group: Analysis Group received research grant from Novartis Pharmaceuticals, Employment. Sasane:Novartis Pharmaceuticals: Employment. Paley:Novartis Pharmaceuticals: Employment. Duh:Analysis Group: Analysis Group received research grant from Novartis Pharmaceuticals, Employment.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal